Cardiovascular health (“Life’s Essential 8”), risk of depression and anxiety: a prospective cohort study

Introduction
Depression and anxiety are two common mood disorders that severely endanger human health longevity and have become public health issues due to the rapid population aging1,2,3. Identifying risk factors and finding implementable intervention measures to prevent the occurrence of mood disorders is a public health priority. However, most of the known risk factors for depression and anxiety, such as genetic factors4, aging5, and childhood adversity6, are difficult or impossible to modify. Several modifiable factors, such as air pollution7 and lifestyle8, have become breakthrough points for preventing the occurrence of anxiety and depression. The extensive body of epidemiologic evidence that cardiovascular diseases (CVDs) are closely related to anxiety and depression9,10, and a bidirectional relationship may exist11.
In 2010, the American Heart Association defined “cardiovascular health (CVH)” based on seven key health factors and behaviors, including diet, physical activity (PA), smoking, body mass index (BMI), blood lipids, blood pressure (BP), and blood glucose to promote individual and population cardiovascular health (“Life’s Simple 7”)12. Over the past decade, CVH was not only widely employed to estimate the risks of cardiovascular events and cognitive health13,14,15, but also the risk of depression. Recently, a prospective community-based cohort of 6,980 participants in France found that better CVH was associated with a lower risk of depressive symptoms over time16. It is in line with a longitudinal analysis of ELSA-Brasil, which included 9214 participants and also suggested that poor cardiovascular health tripled depression risk at follow-up in otherwise healthy adults17. However, previous studies found that “Life’s Simple 7” was not flawless, the ignorance of inter- and intra-individual heterogeneities and the limited capacity of the seven components were noted18,19. Therefore, AHA released a new CVH score named “Life’s Essential 8” in 202219. Components of the new CVH score included updated components for diet, smoking, blood lipids, and blood glucose and additionally included sleep health as the eighth component19. We hypothesized that this updated CVH score could act as a better predictor for the CVD-related risks of late-life depression and/or anxiety.
To examine this hypothesis, we conducted a population-based prospective cohort study to evaluate the associations of the “Life’s Essential 8” with the risk of depression and anxiety. We primarily evaluated the associations of CVH with the risk of depression and/or anxiety and secondarily analyzed whether the genetic preposition of depression/anxiety could modify the relationships between CVH and incident depression/anxiety.
Method
Study population
UK Biobanks is a large population-based prospective cohort study with approximately 500,000 participants. Details of UKB were described in the previous study20. As shown in the flowchart in Supplementary Figure 1, in this study, 447,622 participants with available data on depression/anxiety and CVH scores were included for baseline analysis (analysis 1). The first subset of 388,349 participants who were free of depression or anxiety at baseline was included to evaluate the relationship between CVH and incident depression/anxiety (analysis 2). Among them, a second subset of 129,074 participants who joined a follow-up online mental health survey assessing their mental health including depressive/anxiety symptoms during 2016–2017 was used to evaluate the prospective associations between CVH and the syndromes of depression/anxiety (analysis 3). This subset was further employed in the following symptom analysis. The North West Multicenter Research Ethical Committee has granted the ethics committee approval to the UK Biobank. All participants provided written informed consent at the time of enrollment.
Assessments of depression and anxiety
Mental health questionnaires and hospital admission records (UK Biobank Data-Fields: 41202 and 1204) were linked to the assessment of depression/anxiety. Detailed assessment was reported in our previous article7. Briefly, depression or anxiety was considered positive if the participants’ either record was positive. Considering that anxiety and depression often coexist21, either disorder was defined as participants who experienced either anxiety, depression, or both if the participants posed positive records for depression/anxiety. Co-incident symptoms were defined as participants who simultaneously developed depression and anxiety during the follow-up. Participants were assessed by using both the mental health survey and the hospital records in analyses 1 and 2. Participants from the second subset were assessed only by using the online follow-up mental health survey in analysis 3. For hospital records, participants were classified as cases if they had either an ICD-9/10 code of primary or secondary diagnosis for depression (ICD-9: 311; ICD-10: F32–F33) and/or anxiety (ICD-9: 300; ICD-10: F40–F41). For questionnaire screening, at baseline, the Patient Health Questionnaire (PHQ)-4 questionnaire22 (consisting of 4 items including a 2-item depression scale and 2-item anxiety scale) was used to evaluate depression and anxiety. At 7-year follow-up, depression, and anxiety symptoms were assessed using PHQ-9 (consists of 9 items)23 and generalized anxiety disorder (GAD)-7 (consists of 7 items)24 questionnaires. Participants were required to rate, on a four-point Likert scale from 0 (not at all) to 3 (nearly every day), their response to each item. Therefore, the total score of PHQ-4 ranged from 0 to 12 and a score of ≥6 was considered emotional disorder positive. A total score of ≥3 on the depression scale was considered as positive for depression, and a total score of ≥3 on the anxiety scale was considered as anxiety positive22. Total scores of PHQ-9 and GAD-7 ranged from 0 to 27 and 0–21, and the PHQ-9 or GAD-7 total score of ≥10 was considered as depression or anxiety symptoms positive, respectively23,24. Additionally, any item with a score of ≥1 was considered positive for this symptom.
Covariates
Age, sex, hypertension, ethnicity, healthy alcohol intake, diabetes, Townsend deprivation index, coronary heart disease (CHD), education, and childhood adversity (an additional covariate for sensitivity analyses) were included as covariates. Ethnicity, healthy alcohol intake, education, history of hypertension, diabetes, and CHD were based on self-reported information and medical records. Ethnicity was categorized into White, Black, Asian, and other. Healthy alcohol intake status was defined as: female: <14 g/day and male: <28 g/day; The medical history of hypertension, CHD, and diabetes was obtained from self-reports and medical records; The Townsend deprivation index, calculated using four variables from the UK Biobank dataset (unemployment, overcrowded household, non–car ownership, and non–home ownership), indicates the level of deprivation, with a higher index indicating a higher level of deprivation; Years of education was classified into <10 years and ≥10 years. Adverse childhood experiences and early Trauma are associated with worse CVH in adults and are risk factors for depression/anxiety across the life-course25,26. We examined whether childhood adversity could affect the associations between CVH and incident depression/anxiety, as part of sensitivity analyses. Detailed assessments of childhood adversity were described as supplementary methods.
Quantification of CVH score
The CVH score of each participant at baseline was calculated, including diet, PA, smoking, sleeping, BMI, blood lipids, blood glucose, and BP according to the AHA algorithm. Each participant’s score scored on a scale of 0–100 points and the total score was calculated by summing the scores for each of the eight components together19. The total score was classified into two subgroups including health behaviors (smoking, PA, sleeping, diet) and health assessments (BMI, blood glucose, BP, and blood lipids). Additionally, a 7-item CVH score based on the “Life’s Simple 7” components without the component of sleep health was calculated by summing the scores of diets, PA, smoking, BMI, blood lipids, blood glucose, and BP. Detailed measures of each score were described in supplementary methods.
Polygenic risk scores
We measured background genetic risk for depression/anxiety disorders using polygenic risk scores (PRS) for depression, anxiety, and a combined depression/anxiety phenotype. Detailed measures of PRS were described in supplementary methods. The best-fitting parameters for the PRS for depression, anxiety, and both disorders were demonstrated (Supplementary Table 1). The resulting PRSs explained of 7.55–8.34% of variance in the odds of depression, and anxiety, either disorder, and the PHQ-4 score at baseline (Supplementary Table 2).
Statistical analyses
First, the associations of CVH with PHQ-4 scores and the prevalence of depression/anxiety at baseline were examined by linear regression and logistic regression at baseline, respectively (analysis 1). Two models increasingly adjusted for potential covariates: Model 1 controlled for age, and sex. Model 2 increasingly adjusted for hypertension, ethnicity, healthy alcohol intake, diabetes, CHD, Townsend deprivation index, and education. Dose–response curves were assessed by restricted cubic spline regression models27 controlling for all potential covariates, with the 25th, 50th, and 75th percentiles of CVH score selected as knots. Additionally, to determine whether the new scores had better predictive power, the associations of the revised 7-item CVH score with the odds of depression and/or anxiety were also examined at baseline as a sensitivity analysis.
Second, the time-to-event analysis between the baseline CVH score and the risk of either disorder, depression, and anxiety at follow-up (the first subset) were tested by using hazard ratio [HR] with 95% confidence intervals [CI] from Cox proportional hazards models (analysis 2). Dose–response relationships related to the risk of the incident, either disorder, depression, or anxiety, were further assessed by the restricted cubic spline regression. The association between CVH score and the co-incidence of depression and anxiety was also evaluated using a competing risk regression model. Subsequently, we tested the prospective associations of the baseline CVH score with the scores of PHQ-9 and GAD-7 and the detailed symptoms of depression/anxiety using linear regression and logistic regression in the second subset of participants with 7-year follow-up data (analysis 3). The aim of this analysis was to evaluate the associations of baseline CVH with the syndromes of depression/anxiety to additionally provide insights into CVH on mental disorders. Similarly, to test whether the new scores had better predictive power, the associations of the revised 7-item CVH score with the risk of depression and/or anxiety were additionally examined as another sensitivity analysis.
We performed three sensitivity analyses to test the robustness of our above findings. First, we examined whether age and sex could interact with CVH in the associations between CVH and the risk of depression/anxiety and the prediction of co-incident depression and anxiety. Then, we tested whether early-life childhood adversity could affect the associations between CVH and incident depression/anxiety among 125,358 participants free of depression/anxiety at baseline with available childhood adversity data retrieved from a follow-up survey. Last, we performed another sensitivity analysis of the second step analysis by excluding participants who were followed for ≤2 years to avoid reversal causality.
Finally, to explore the interactions between the genetic risk of depression/anxiety and CVH score on the incidence of depression/anxiety, we tested the interaction between the CVH score and PRS using the primary Cox proportional hazards model by adding an interaction term of the two factors. In the case that the interaction effect met the criteria for statistical significance, we generated a 16-level categorical variable based on the quartiles of CVH score and PRS. The fourth quartile (Q4) of CVH score and the first quartile (Q1) of PRS were combinedly defined as level 1 for the lowest risk of depression/anxiety, and Q1 of CVH score and Q4 of PRS were combined as the highest risk group accordingly. Associations of the new 16-level variable with the risk of depression/anxiety were evaluated using the Cox model.
R version 4.0.5 (R Development Core Team, Vienna, Austria) and SAS version 9.4 TS1M7 (SAS Institute Inc., Cary, NC, USA) were used for data cleaning and all analyses. P-values from the two-sided of <0.05 were considered statistically significant.
Results
Characteristics of participants
As shown in Table 1, at baseline, all participants’ average age (mean ± SD) and CVH score were 56.51 ± 8.07 years and 538.72 ± 93.14, 45.0% were men, 49.41% had drunk alcohol, 54.2% were never smokers, and most of them (95.4%) were white. In the hand of major chronic diseases, 27.3% of participants had prevalent hypertension, 5.6% had prevalent CHD, and 5.1% had prevalent diabetes. At baseline, the average PHQ-4 score was 1.61 ± 2.11. About 13.2%, 10.6%, and 6.5% of participants were diagnosed with either disorder, depression, or anxiety based on PHQ-4 scores and hospital records, respectively. In the first subset, 388,349 participants who were free of depression or anxiety at baseline were followed up for a median time of 8.7 years, and the average PHQ-4 score was 0.10 ± 1.18. Among them, 17,554 (4.52%) participants developed either disorder (Ndepression = 11,739; Nanxiety = 8982). In the second subset with the 7-year follow-up, participants’ s averaged PHQ-7 and GAD-7 scores were 2.28 ± 3.06 and 1.75 ± 2.90, respectively. About 6.6%, 4.5%, and 3.6% of participants demonstrated symptoms meeting the criteria of either disorder, depression, or anxiety based on corresponding scores.
Association of CVH score with the odds of depression and/or anxiety at baseline
At baseline, participants had higher PHQ-4 scores and were at higher odds of with symptoms of depression, anxiety, or either disorder when they had lower CVH scores (Table 2, Supplementary Fig. 2). After fully adjusting for potential covariates, per 100-point decrease in CVH score was significantly associated with a 0.3-unit (standard error [SE] = 0.0036) increase in the PHQ-4 score, and with a gradually increased odds of either disorder (odds ratio [OR] = 1.458, 95% CI:1.443–1.473), depression (OR = 1.481, 95% CI:1.460–1.501), and anxiety (OR = 1.487, 95% CI:1.470–1.503). Compared to the highest quartile of CVH score, the group of the lowest CVH score quartile showed a 0.7-unit (SE = 0.0092) increase in PHQ-4 score, and the ORs of either disorder, depression, and anxiety were 2.347 (95% CI: 2.284–2.412), 2.414 (95% CI: 2.324–2.507), 2.478 (95% CI: 2.404–2.554), respectively. Compared to the new score, the 7-item CVH score without considering sleep health had a lower predictive power (Supplementary Table 3).
Association of CVH score with the risk of depression and/or anxiety symptoms during follow-up
As shown in Table 3, for 388,349 participants free of depression/anxiety at baseline, we observed consistent results in crude and fully adjusted models. After fully adjusted, per 100-point decrease in CVH score was associated with an increased risk of incident either disorder (HR = 1.133, 95% CI: 1.114–1.153), depression (HR = 1.205, 95% CI: 1.180–1.231), and anxiety (HR = 1.042, 95% CI: 1.017–1.069), co-incident depression and anxiety (HR = 1.128, 95% CI: 1.083–1.176). Compared to the highest quartile of CVH score, the group of the lowest CVH score quartile was significantly associated with an increased risk of incident events with symptoms of either disorder (HR = 1.341, 95% CI: 1.282–1.403), depression (HR = 1.553, 95% CI: 1.470–1.641), and anxiety (HR = 1.106, 95% CI: 1.038–1.177), co-incident depression and anxiety (HR = 1.337, 95% CI: 1.204–1.485). Compared to the new score, the 7-item score had lower predictive power (Supplementary Table 4).
Additionally, significant associations were observed between the risk of all outcomes and components of CVH (Supplementary Table 5). For instance, per 20-point decrease in the smoking score was significantly associated with an increased risk of incident either disorder (HR = 1.106, 95% CI: 1.095–1.116), and per 100-point decrease in health assessments or health behaviors was significantly associated with an increased risk of incident either disorder (HRhealth assessments = 1.085, 95% CI: 1.058–1.113, HRhealth behaviors = 1.217, 95% CI: 1.186–1.250). We further observed monotonic increasing trends that the decreased CVH score (including total, health behaviors, and health assessments) was positively associated with a higher risk of all outcomes, except the marginal association between the health assessment score and incident anxiety (Fig. 1).
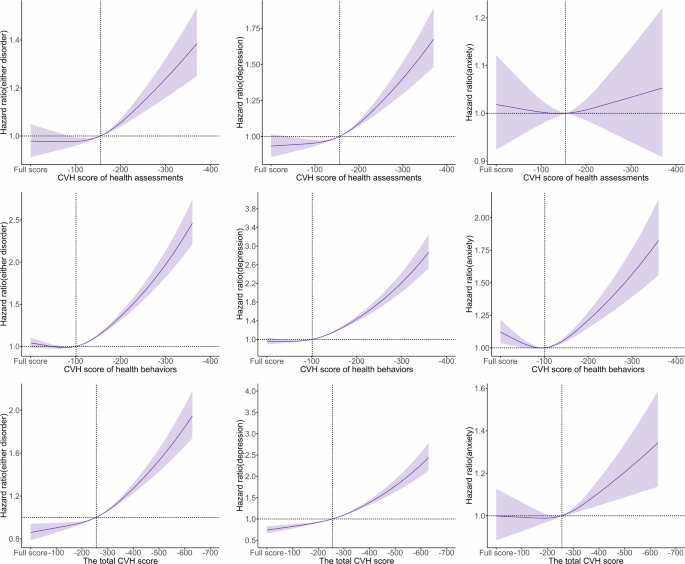
Solid line: Point estimation; Shadows: Confidence limits; Dash line: Reference line; The CVH score of health assessments (0–400 points) was calculated based on four components of health assessments (BMI, blood glucose, BP, and blood lipids). The CVH score of health behaviors (0–400 points) was calculated based on four components of human behaviors (smoking, PA, sleeping, and diet). The total CVH score (0–800 points) was calculated based on all components. The restricted cubic spline regression model adjusted for age, sex, ethnicity (White, Black, Asian, and other), healthy alcohol intake(yes/no), years of education (<10 years), Townsend deprivation index, prevalent hypertension, CHD, and diabetes (yes/no). CHD coronary heart disease; Full-score = 400/800 points.
Association of CVH score with the odds of depression and/or anxiety symptoms at 7-year follow-up
Among 120,974 baseline depression/anxiety-free participants with detailed symptoms at the 7-year follow-up, they presented higher PHQ-9 and GDA-7 scores and were more easily with depression, anxiety, either disorder at the 7-year follow-up when they had lower CVH score at baseline (Supplementary Table 6). Per 100-point decrease in CVH score was significantly associated with 0.36 unit (SE = 0.0102) increase in the PHQ-9 score and 0.10 unit (SE = 0.0097) increase in the GDA-7 score and with a gradually increased odds of either disorder (OR = 1.264, 95% CI: 1.231–1.298), depression (OR = 1.371, 95% CI: 1.329–1.414), and anxiety (OR = 1.136, 95% CI:1.097–1.176). Compared to the highest quartile of CVH score, the group of the lowest CVH score quartile was significantly associated with the increased odds of either disorder (OR = 1.637, 95% CI: 1.533–1.749), depression (OR = 1.999, 95% CI: 1.846–2.165), and anxiety (OR = 1.325, 95% CI: 1.208–1.454). CVH score also was associated with each symptom of depression and anxiety (Fig. 2).
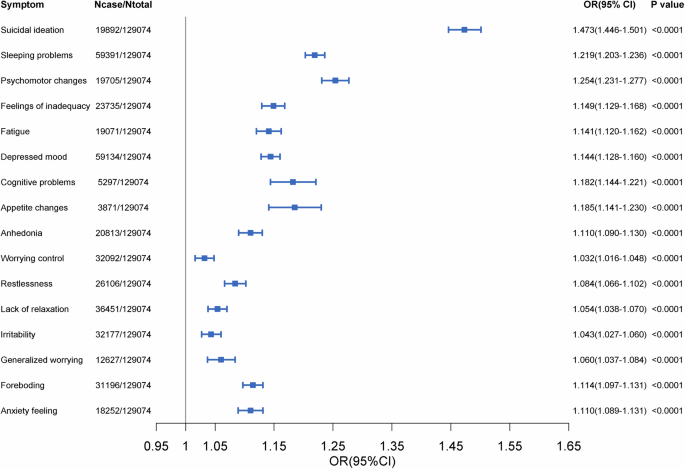
Models adjusted for age, sex, ethnicity (White, Black, Asian, and other), healthy alcohol intake(yes/no), years of education (<10 years), Townsend deprivation index, prevalent hypertension, CHD, and diabetes (yes/no). Estimates of CVH were demonstrated per 20-point decrease. Dots: Point estimate; Error bar: 95% confidence limits.
Three sensitivity analyses were performed to test the robustness of our above findings. First, we did not observe the interaction of sex and age with CVH in the associations between CVH and the risk of depression/anxiety and the prediction of co-incident depression and anxiety (all P-interaction > 0.05, Supplementary Table 7). Then, since we considered whether childhood adversity might affect CVH and incident depression/anxiety, we repeated the analysis of incident depression/anxiety in the subset of participants who were free of depression/anxiety at baseline and who participated in the follow-up online survey that collected reports of childhood adversity (N = 125,358). After adjustment for childhood adversity, effect sizes for CVH were similar to effect sizes from our primary analyses of incident depression/anxiety (Supplementary Table 8). Finally, we repeated the analysis in participants who were followed for >2 years to avoid reversing causality. Similarly, we observe a robust association between CVH and the risk of depression/anxiety (Supplementary Table 9).
Joint effects of CVH score and genetic susceptibility on depression/anxiety
Finally, we found that the interactions between CVH score and PRS were not significant for either disorder (P–interaction = 0.5471), depression (P–interaction = 0.5248), and anxiety (P–interaction = 0.3638). However, the 16-level variable was then generated according to each health outcome, and we observed that compared with the lowest risk level (Q4 of CVH score and Q1 of PRS), participants showed elevated risks of depression/anxiety by the increasing risk levels (Supplementary Fig. 3). For those with the highest risk (Q1 of CVH score and Q4 of PRS), the HRs were 1.313 (95% CI: 1.205–1.431), were1.380 (95% CI: 1.240–1.537) and were 1.255 (95% CI: 1.117–1.411 for either disorder depression and anxiety, respectively (Supplementary Table 10).
Discussion
In this prospective cohort study, we evaluated the associations of the updated CVH score with prevalent and incident depression and/or anxiety symptoms. Our findings suggested that adults with poorer CVH were more likely to experience depression and/or anxiety in late-life compared with those who had better CVH at baseline. The associations between CVH score and increased risk for depression and either disorder symptoms are mildly modified by the genetic background captured by PRS. To the best of our knowledge, this is the largest prospective cohort study that revealed the association of the redefined “Life’s Essential 8” CVH score with depression/anxiety.
Several previous studies have examined the relationship between the “Life’s Simple 7” CVH and depression11,17,28. Our results were consistent with these studies. For instance, a prospective cohort study from ELSA-Brasil found that poor CVH tripled depression risk at follow-up in otherwise healthy adults17. Beyond revealing the identical association between CVH and depression in line with these investigations, our study also studied the relationship of CVH score with anxiety and its co-incidence with depression. Although the genetic risk of depression/anxiety did not interact with the CVH score, only a mild modifying effect in the joint analysis, we look forward to a better characterization of depression/anxiety risk with more novel SNPs identified by upcoming GWASs.
More intriguingly, we compared the primary findings with a 7-item CVH score without component sleeping in the sensitivity analyses. We did not observe an association between the 7-item CVH score and the risk of incident anxiety, and the 7-item CVH score had reduced predictive efficacy for prevalent and incident depression and/or anxiety. Consistently, we found that the score of sleeping health appeared to have the most robust association with depression and/or anxiety in all components, suggesting that sleep quality plays a central role in linking CVH with depression/anxiety. This additionally poses another rationale for adding sleep quality to the updated CVH score, as discussed by the AHA Presidential Advisory19. Many environmental factors, such as air pollution, can lead to changes in sleep/circadian systems via biological changes including DNA methylation29. Evidence indicates that sleep/circadian are closely related to serotonin, a neurotransmitter30, which is an important target in the treatment of depression and anxiety31. Therefore, it is reasonable to speculate that changes in sleep may lead to the occurrence of anxiety and depression by affecting the levels of certain neurotransmitters.
For other components of CVH, we generally found consistent associations except for BP and diet. In our study, participants with higher BP scores, i.e., better blood pressure, had higher risks of developing anxiety and depression. However, a cross-sectional study showed that participants with ideal BP had a 79% increase in the odds of depression compared to those with poor BP32. One of the possible mechanisms for this result is that neurons that could control BP may express neuropeptide Y may play a role in lowering BP and inducing anxiety33. Additionally, the associations between depression and/or anxiety and CVH components appeared to be stronger for the CVH behaviors (PA, smoking, sleeping, and diet) than the components of health assessment. A similar trend was also observed in two previous studies28,34. For example, Zhang, Z et al. found a graded association between CVH, particularly for health behaviors, and mild and moderate/severe depression among U.S. adults. Altogether, these results suggest that compared with the components of health assessments, CVH-related health behaviors weigh more in leading to depression/anxiety. In addition to the sleep behaviors discussed earlier, regular PA could offer substantial benefits for public mental health35. Consistent exercise boosts the production of kynurenine aminotransferase in muscles, leading to a favorable shift in the balance between the neurotoxic kynurenine and the neuroprotective kynurenic acid, thereby reducing the risk of developing mental disorders36. Growing evidences also suggested that dietary interventions could serve as a complementary approach to treating mental disorders37. A previous review has highlighted various mechanisms through which diet may influence mental health, including modulation of inflammation, oxidative stress, mitochondrial function, gut microbiota, tryptophan–kynurenine metabolism, the hypothalamic–pituitary–adrenal axis, neurogenesis, brain-derived neurotrophic factor levels, epigenetics, and obesity38. A large body of evidence has reported that these behavioral changes could potentially trigger anxiety and depression by impacting neurotransmitter levels, the plasticity of neurons, and stress responses, within the brain, as well as altering levels of some inflammatory cytokines39,40,41. In summary, daily behavioral interventions could be an essential approach for preventing mental disorders.
Our study has strengths including the large sample size and the detailed records for constructing the CVH score. We also assessed the background genetic risk for depression/anxiety using PRS leveraging the rich genetic data of UK Biobank. However, we also acknowledge several limitations of this study. Firstly, participants tending to be healthier and wealthier from the UK Biobank do not represent the UK population as a volunteer cohort42,43. Relatively healthier and wealthier participants may suffer from less psychosocial pressure. Early-life experiences of mental health problems may also change a person’s tendency to have a bad CVH44. Secondly, smoking, PA, diet, sleeping, and alcohol use were self-reported and subject to misclassification and recall biases. Especially the diet score was modified due to the lack of sodium direct relevant data that was instead by salt added to food. We also look forward to more studies in the future using actigraphy measures for a more objective evaluation of CVH metrics, such as sleep and PA. Meanwhile, for the assessment of anxiety and depression, we exclusively relied on questionnaires and medical records. However, given the underestimation and underreporting of mental health issues in older adults is common45, more precise and comprehensive diagnoses of mental disorders are recommended in future studies. Thus, the association of CVH with depression and/or anxiety might be over- or under-estimated to some extent. Furthermore, with the limited follow-up, clinically significant changes in CVH components during the follow-up were not comprehensively recorded. This potential bias may lead to the underestimation of the prediction of CVH score on depression/anxiety. Besides, Our analysis did not adjust for medication use that could potentially influence the association between CVH and depression/anxiety, due to the lack of this information. Given our follow-up data was retrieved primarily from links to electronic health records, we believe that most included participants were treated appropriately throughout the study period once diagnosed. Finally, as only about 1/3 of participants joined in the 7-year survey and we observed a larger proportion of participants with depression/anxiety in this subset than the whole participants without depression/anxiety at baseline, the real-world burden of depression and anxiety during the follow-up could be worse than that based on the current information.
In conclusion, we found that adults with worsened cardiovascular health showed an elevated risk of incident events with depression/anxiety symptoms. Under the circumstances of population aging, our findings shed light on the approach that we can promote the health of cardiovascular systems from midlife through healthy behavioral interventions to reduce the late-life incidence of depression/anxiety. This could present on path to reducing the social burden of depression/anxiety.
Responses