Understanding endometriosis underfunding and its detrimental impact on awareness and research

Introduction
Endometriosis, a chronic disease defined by the presence of endometrium-like tissue outside the uterus, affects approximately 190 million women* globally1. It is associated with a range of often debilitating symptoms, including severe pelvic pain, bowel and bladder symptoms, fatigue, and risk of infertility2,3. Despite its high prevalence, diagnosis is delayed on average by 7–9 years, and this has remained consistent over the past ten years, with effective therapy and care frequently falling short4. Research conducted by the Finding Endometriosis using Machine Learning (FEMaLe) Project has shed light on the significant underdiagnosis of endometriosis. In Denmark, only up to 2% of women in the reproductive age receive a diagnosis5, compared to an estimated 10%, despite that individuals with endometriosis use the Danish healthcare system 19% more often than those without the condition, in the ten years preceding the diagnosis6. The consequences of this diagnostic delay are numerous. First, without adequate treatment, the disease may progress, becoming increasingly difficult to manage. Existing symptoms, such as pain, may become chronic, and new symptoms may develop over time2,3,4. Second, the psychosocial impact of this ‘medical merry-go-round’, as some patients describe it, can significantly reduce the quality of life for those with endometriosis. This includes poor mental health, as well as challenges in interpersonal relationships and occupational settings7,8. Many people with endometriosis face complex journeys to and through care9, which exist within a broader context of historically under-funded research into women’s health and chronic pain10. A recent study documented the significant underinvestment in endometriosis research projects across the European Union’s framework programmes, where a staggering low 27 out of 145,983 projects funded in total (0.02%) were found to be related to endometriosis11. This lack of financial support perpetuates a cycle of knowledge gaps and limited awareness, contributing to delayed diagnosis and inadequate treatment options for those affected. In this article, we will explore the multifaceted ramifications of underfunding in endometriosis research, comparing it to diseases with similar prevalence and impact, namely diabetes and inflammatory bowel disease12,13. We will discuss its detrimental effects on awareness and scientific advancements, highlighting the urgent need for increased investment in innovative tools and methods to propel research and innovation forward.
Comorbidities, costs, and consequences: the underfunding dilemma
Systematic reviews and meta-analyses have shown that women with endometriosis have higher rates of co-occurrence of gastrointestinal diseases (such as irritable bowel syndrome and inflammatory bowel disease, immunological diseases (such as rheumatoid arthritis and psoriasis), and cardiovascular diseases (such as coronary heart disease, hypercholesterolemia, and hypertension) compared to women without endometriosis10,14. The estimated annual cost of endometriosis per affected woman is €9500, attributed to loss of productivity and direct healthcare costs. This is similar to the costs associated with diabetes and Crohn’s disease15,16. The National Institutes of Health (NIH), the largest source of biomedical research funding globally, allocates nearly $48 billion USD annually to the study of various diseases and conditions17. In 2022, the total US funding for endometriosis was $16 million (0.038%), which translates to $2.00 per patient per year. By comparison, 12% of US women are expected to suffer from diabetes in their lifetime. Assuming that half of the diabetes research budget will be allocated to female patients, this results in $31.30 per woman per year. Similarly, Crohn’s disease impacts over 690,000 people in the US. In 2022, Crohn’s disease research received $90 million in funding, which is $130.07 per patient, over 65 times more per patient than for endometriosis18. This illustrates that despite its significant disease burden, endometriosis receives disproportionately less research funding compared to other chronic conditions with similar high prevalence and impact19, such as diabetes and inflammatory bowel disease. The estimated socioeconomic burden of endometriosis has been criticised for potentially being too conservative, meaning that the true disparity between disease burden and funding could be even greater20.
Impact on awareness
Investments in public health awareness campaigns, educational initiatives, and menstrual health literacy programs are crucial for dispelling myths, reducing stigma, and empowering individuals to seek timely medical attention. However, the absence of financial support for awareness raising activities contributes to a pervasive lack of understanding and recognition of endometriosis among the general population, healthcare professionals, and policy-makers alike21. Moreover, many individuals with endometriosis experience delays in diagnosis due to the normalisation of menstrual pain and the dismissal of their symptoms as ‘routine’ discomfort22. The stigma and taboo surrounding menstruation and reproductive health perpetuates a culture of silence and shame, hindering open dialogue about endometriosis23. Ultimately, current knowledge and research merely underlines how underfunding is reflecting a broader societal attitude towards women’s health issues and menstrual disorders, maintaining a cycle of neglect and marginalisation. To explore the current state of awareness in Denmark, we have searched Infomedia, a media intelligence powerhouse in the Nordics, to assess endometriosis’ media coverage compared to diabetes and inflammatory bowel disease in Denmark from 1992 to 2023. We found that ‘diabetes’ has been mentioned almost 77 times more often (n = 201,255) than ‘endometriosis’ (n = 2621), whereas ‘inflammatory bowel disease’, including ‘Crohn’s’ and ‘colitis ulcerosa’, has been featured almost twice as much (n = 4384). By raising awareness of endometriosis as a legitimate medical condition deserving attention and resources, we can facilitate earlier diagnosis, improve treatment outcomes, and ultimately alleviate the burden of disease for millions worldwide1,24.
Exploring endometriosis funding in Denmark
We have assessed the top 100 grant-awarding foundations in Denmark25 to compare their support in (research) projects on endometriosis, diabetes (mellitus type 1 and 2), and inflammatory bowel disease until 2023. In total, 9 foundations have supported one or more of the three conditions illustrated by fed back data or published information about grant awards, as shown in Fig. 1. Our Danish investigation demonstrates that when comparing the total grant-awarded endometriosis research projects (173,958 EUR) with those on diabetes (254,908,430 EUR) and inflammatory bowel disease (325,940 EUR), endometriosis remains severely underfunded.
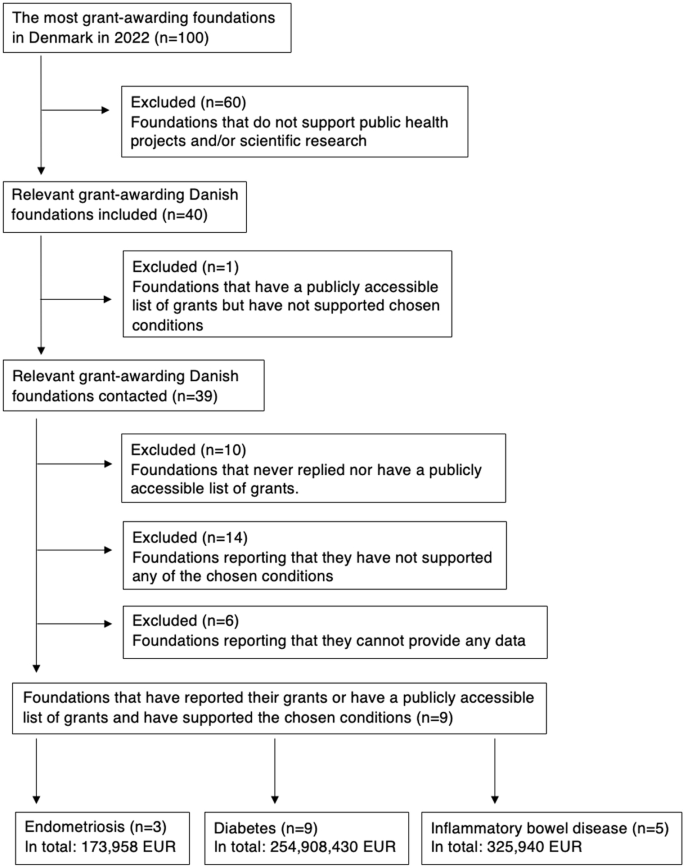
This figure presents the funding distribution from the top 100 grant-awarding foundations in Denmark, supporting research projects on endometriosis, diabetes (mellitus type 1 and 2), and inflammatory bowel disease until 2023. Of these foundations, only nine have provided support for one or more of the three conditions, as illustrated. Our analysis reveals a significant funding disparity, with endometriosis research receiving 173,958 EUR in grants compared to 254,908,430 EUR for diabetes and 325,940 EUR for inflammatory bowel disease. These findings underscore the underfunding of endometriosis research relative to other chronic conditions.
Hindrance to research advancements
Endometriosis research faces significant barriers due to chronic underfunding, limiting the scope and depth of scientific inquiry into the disease’s underlying mechanisms and potential therapeutic interventions. More basic research into the pathophysiology of endometriosis is essential for elucidating the complex interplay of genetic, hormonal, and environmental factors contributing to disease development and progression26. However, limited funding impedes researchers’ ability to conduct large-scale epidemiological studies, genetic analyses, molecular and mechanistic investigations necessary for advancing our understanding of the condition. Moreover, the severe lack of financial support for international and interdisciplinary research collaborations, such as the FEMaLe Project, hampers progress towards developing targeted therapies and personalised treatment strategies for endometriosis. Without adequate resources, researchers struggle to translate scientific discoveries into clinical applications, thereby increasing the knowledge gap between benchtop research and bedside care. Investment in endometriosis research is not only essential for improving patient outcomes but also holds promise for uncovering insights into related conditions such as infertility, pelvic pain disorders, and certain types of cancer10,24. By prioritising funding for endometriosis research, policymakers and funding agencies can catalyse cutting-edge scientific advancements, drive innovation, and ultimately improve the lives of millions affected by this complex and often debilitating condition21,26.
The urgent need for increased investment
Addressing the significant underfunding of endometriosis requires a concerted effort from policymakers, funding agencies, and advocacy organisations. Investing in endometriosis research and awareness initiatives is not only a matter of scientific priority but also a question of social justice and gender equity. Women disproportionately bear the burden of endometriosis, yet their healthcare needs remain chronically underfunded and overlooked19,20. By prioritising investment in women’s health research, policymakers can advance gender equity in healthcare and address longstanding disparities in funding and resource allocation11,18,19. Moreover, increased investment in endometriosis research has the potential to yield significant economic and societal benefits8,15,16. By improving diagnosis and treatment outcomes, we can reduce healthcare costs associated with the management of endometriosis-related complications and comorbidities. Investing in innovative research approaches and digital health development can also stimulate scientific innovation, foster academic collaboration, and strengthen the competitiveness of research institutions24.
Conclusion
In this article, we investigated the funding of endometriosis compared to irritable bowel syndrome and diabetes in a Danish setting, similar to a previous comparison conducted in the US18. The significant underfunding of endometriosis perpetuates a cycle of knowledge gaps, suffering, and missed opportunities for scientific advancement. To address this urgent issue, we must prioritise endometriosis research and advocacy efforts, allocating resources commensurate with the disease’s prevalence and impact. By raising awareness, fostering interdisciplinary collaboration, and investing in innovative research initiatives, we can pave the way for a brighter future for those affected by endometriosis. It is time to recognise endometriosis as a global health priority and take decisive action to drive positive change. Only through collective effort and investment can we unravel the enigma of endometriosis and improve the lives of millions worldwide.



Responses