Female sexual response among Flo app users in the United States

Introduction
Female sexual response is multidimensional and characterized by various factors, including desire, arousal, and orgasm, that collectively contribute to an individual’s sexual experience and satisfaction1,2. Evidence shows the importance of sexual satisfaction, with 62.2% of men and 42.8% of women in the United States placing a high value on sexual satisfaction for quality of life3. Yet, an estimated 43.1% of women in the United States experience sexual problems, with 22.2% experiencing sexually related personal distress4.
Impaired female sexual response can take on different forms, including a disruption in sexual desire, difficulties with arousal, and challenges achieving orgasm5. If this impairment affects an individual’s ability to participate in desired sexual relationships, persisting for a minimum of 6 months and causing clinically significant distress, it is termed female sexual dysfunction (FSD)6. FSD can be characterized by multiple disorders, namely hypoactive sexual desire disorder, sexual aversion disorder, female genital arousal disorder, persistent genital arousal disorder, female orgasmic disorder, pleasure dissociative orgasm disorder, female orgasmic illness syndrome, or sexual pain disorders7. FSD is underdiagnosed and undertreated by clinicians8. Even in the absence of clinically diagnosed sexual dysfunction, women report lower sexual satisfaction. In a 2017 study of over 2000 participants across the US without diagnosed sexual dysfunction, only 49.4% of heterosexual women reported satisfaction with their sex lives9.
Female sexual response is complex and can be affected by multiple factors, such as age10, use of medication11, physical and emotional health, negative sexual experiences, and length of relationships12,13. Partner factors, such as conflict, partner’s sexual function, and fertility-focused intercourse, also play an important role14. Sexual response also appears to be associated with life phases, including during pregnancy and postpartum15, and peri/postmenopause16. In most existing investigations of female sexual response, the average age of participants tends to be in the mid-40s, which limits generalizability since menopause and comorbid health conditions affect sexual response17. Investigations in younger women are often in the context of comorbid conditions such as Polycystic ovary syndrome (PCOS) and endometriosis, thus leaving female sexual response relatively understudied in healthy reproductive-aged women18.
Updated population-level reports of female sexual response in demographically diverse populations are needed to properly contextualize sexual disorders and inform care. Technology-based interventions via mobile applications have become increasingly popular for tracking the menstrual cycle, ovulation, and related events important for reproductive well-being. Such applications can offer unique opportunities for examining sexual function at a population level given the ease of use, accessibility, and anonymity19,20. Flo Health Inc. is one such period and ovulation tracking application (app). The app is available in both free and subscription forms through iOS and Android platforms. Flo facilitates period and ovulation tracking, provides symptom-tracking functionality, evidence-based educational content, health assistants to check symptoms against various health conditions as well as so-called “Secret chats” for anonymous peer-to-peer engagement between users.
In this study, we sought to estimate female sexual response, using female sexual function index (FSFI-6), among a large and demographically diverse sample of users of the Flop app in the United States. We also aimed to evaluate associations between sexual response and different sociodemographic characteristics, health conditions, and logging of sex events in the Flo app.
Results
Descriptive analysis
The mean FSFI-6 score was 22.5 out of a possible 30, with a Cronbach’s alpha of 0.731 (Table 1). The highest score was in the pain domain (mean = 4.3). For the pain domain, higher scores suggested less pain. Participants scored lowest in the desire and orgasm domains (3.4 each). Among the 2392 study participants, only 11 (0.5%) participants had received an FSD diagnosis.
Sociodemographic analysis
Participants who acknowledged trying to conceive scored significantly higher on the FSFI-6 (representing better sexual function) compared with those who were using Flo to only track their cycle (Difference: 0.83; 95% confidence interval (CI) 0.43 to 1.23) (Fig. 1a and Supplementary Table 1). Having obesity was also associated with better sexual function as reflected in higher FSFI-6 scores (0.58; 95% CI 0.13 to 1.03), and conversely, being underweight was associated with lower sexual function as represented by lower FSFI-6 score (−1.35; 95% CI −2.44 to −0.26) compared to not being underweight. Being 35 or older was associated with higher domain scores for orgasm and pain, but lower domain scores for satisfaction.
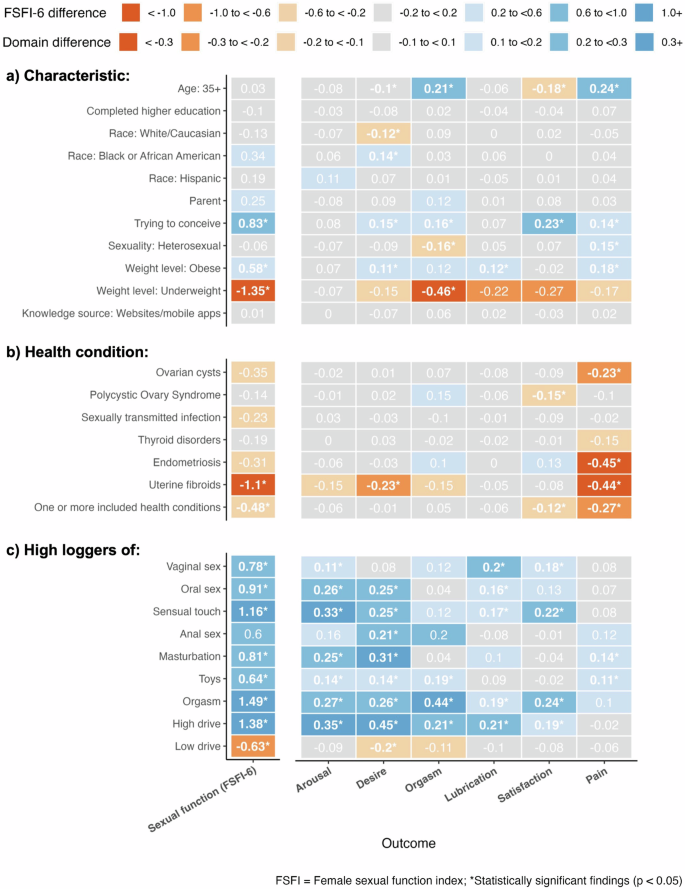
Differences are provided in three panels representing the three groups of predictors used in the analysis: a) population characteristic; b) health condition; and c) logging of sex events.
Health condition analysis
Reporting at least one of the included health conditions was associated with lower FSFI-6 scores (Difference: −0.48; 95% CI −0.85 to −0.11), as well as lower pain scores (meaning more pain) (-0.27; 95% CI −0.35 to −0.19) and lower satisfaction scores (−0.12; 95% CI −0.22 to −0.03) (Fig. 1b and Supplementary Table 2). This finding appears to be driven by uterine fibroids, the only condition when analyzed in isolation, that was associated with lower FSFI-6 scores (−1.1; 95% CI −2.03 to −0.16). Among the FSFI domains, pain was most strongly associated with the included health conditions, with lower domain scores for endometriosis (−0.45 95% CI −0.62 to −0.27), uterine fibroids (−0.44 95% CI −0.64 to −0.23), and ovarian cysts (−0.23 95% CI −0.34 to −0.12). Women with PCOS also had lower domain scores for satisfaction (−0.15 95% CI −0.30 to 0.00), and women with uterine fibroids had lower domain scores for desire (−0.23 95% CI −0.44 to −0.02).
Logging analysis
Of 2392 study participants, 2095 (87.6%) used the in-app symptom, activities, and events logging panel (Supplementary Table 3). Non-sex events (physical symptoms, physical activity, and mood symptoms) were logged on average 4.2 times per week in the year preceding survey completion. Vaginal sex was the most frequently logged sex event (average logs over the previous year: 23.0), followed by high sex drive (6.5) and masturbation (3.8).
Users who logged higher than average vaginal sex events had higher FSFI-6 scores compared with users who logged vaginal sex at or below the population average (Difference 0.78; 95% CI 0.35 to 1.22) (Fig. 1c and Supplementary Table 4). High logging of orgasms (1.49; 95% CI 1.04 to 1.94), high sex drive (1.38; 95% CI 0.89 to 1.88), and sensual touch (1.16; 95% CI 0.60 to 1.72) were most strongly associated with higher FSFI-6 scores. High logging of oral sex (0.91; 95% CI 0.38–1.45), masturbation (0.81; 95% CI 0.31 to 1.31), and toys (0.64; 95% CI 0.15 to 1.14) were also positively associated with FSFI-6 scores. High logging of low sex drive was negatively associated with FSFI-6 scores (−0.63; 95% CI −1.10 to −0.15).
High logging of high sex drive and orgasms most strongly associated with different FSFI domains (Fig. 1c). There was limited association, except for high logging of masturbation and toys, between the included sex events and experiencing pain during sexual intercourse. Anal sex was the only included sex event that was not associated with FSFI-6 scores.
Discussion
In this study, we estimated female sexual response using the FSFI-6 in a large and demographically diverse sample of users of the Flo Health mobile application in the United States. We also evaluated associations between sexual response and different sociodemographic characteristics, health conditions, and logging of sex events. The highest sexual function score was noted in the pain domain (mean = 4.3 out of a possible 5), indicating relatively low pain levels. The lowest scores were in the desire and orgasm domains (mean = 3.4 each), suggesting the lowest level of sexual function was found in these domains.
Trying to conceive was associated with higher FSFI-6 scores (Fig. 1a). Previous evidence on associations between trying to conceive and female sexual function has primarily shown trends to the contrary. Studies have suggested that timed sexual encounters with respect to ovulation, which may be stress-provoking, are associated with lower sexual function21,22. Notably, these studies had focused on women diagnosed with infertility. Our study, however, did not collect data on fertility and thus may include women with and without infertility which could explain this difference. We hypothesize that trying to conceive may have been positively associated with higher FSFI-6 scores because of additional motivating factors for intercourse beyond physical and emotional intimacy and pleasure. This is supported by recent data revealing similarly high FSFI overall scores in couples trying to conceive via assisted reproductive techniques versus spontaneous conception23.
The positive association of obesity with higher FSFI-6 scores in our study population (Fig. 1a) was surprising as it is the opposite to what has been seen in previous literature24. In contrast, there was a strong inverse association between being underweight and sexual function, which is supported by previous studies in patients with disordered eating25. Additionally, because being underweight can have negative consequences for reproductive health, given hypothalamic-pituitary-axis dysfunction, it is perhaps unsurprising that this would extend into sexual function26.
Notably, there was no association between overall FSFI-6 scores and age (being under or over 35 years old) in our study group. Previously published data is mixed regarding whether sexual function improves or declines with age4,27,28,29. However, our results are encouraging for female sexual function after age 35 and before reaching postmenopausal age, as evidence suggests a curvilinear relationship between age and rating sexual health with high importance in the mid-30s to mid-40s compared with older and younger populations3.
Reporting at least one of the included health conditions was associated with lower FSFI-6 scores (Fig. 1b), as has been previously reported30,31. Surprisingly, among the individual health conditions, uterine fibroids were the only ones associated with lower FSFI-6 scores. While this has previously been documented, due to other considerations such as abnormal menstrual bleeding, infertility, urinary symptoms, and deep dyspareunia, further investigations are needed to assess causality32,33,34. Associations between other included conditions, such as endometriosis and PCOS, and sexual function have previously been suggested35,36,37. However, data from a recent systematic review suggest the association between PCOS and sexual dysfunction may be weaker than previously thought and warrants further investigation38. Lower sexual function from reporting at least one of the included health conditions was driven by pain and satisfaction (Fig. 1b).
Our results suggest that sex event logging may itself be positively associated with FSFI-6 scores for a number of event types (Fig. 1c). The literature on the associations between different sexual acts and sexual function is limited39. In a 2024 study of 110 undergraduate female students, masturbation frequency had a minimal relationship with female sexual function, however having positive feelings regarding masturbation and maintaining a positive genital self-image was positively associated40. Studies suggest that relationship dynamics, sleep, and stress also influence female sexual arousal and response to sexual touch39,41,42. Overall, our study is the first to estimate a positive association between higher vaginal sex events and higher sexual function. This may be explained by a mutual positive feedback relationship between the two. Still, more research is needed to explore the relationship between types of sexual activity and sexual function.
Being over 35 years old was associated with higher domain scores for orgasm and pain and a lower domain score for satisfaction. Previous reports focused on sexual function and age have used different cut-offs or parameters for contextualization (for instance menopause status, age above 40, etc.), however, they show a negative association between age and lubrication and dyspareunia sexual domains13,27. Given the differences between study populations, it is difficult to directly compare our findings with those previously reported, but our study is the first to report a positive association with age and any sexual function domains. Emering evidence suggests that age and sexual function is influenced by many factors, including quality of life, relationship dynamics, body image, and others1,28,43,44.
This study had a large study population of over 2000 participants thus facilitating a comparison of FSFI-6 scores based on multiple participant characteristics. Additionally, this demographically diverse population was inclusive of racial/ethnic groups, different sexual orientations, parity, and reproductive desires. A limitation of this study is that it may have been prone to selection bias since we only sampled users of a menstrual-tracking mobile application. As a result, the study sample is not fully representative of the sexually active menstruating US population, limiting its generalizability. For example, the sample included a disproportionate amount of highly educated participants, with nearly 43% having a higher education degree compared to 33% in the general population among 18-64 year olds45. Our study sample included participants aged 18–54 years, thereby limiting the interpretation of our results to this age group. Our study limited recall bias by utilizing a recall window of four weeks, which has been suggested as an acceptable recall period for many aspects of sexual function46. However, as a result, participants needed to be sexually active in the four weeks preceding survey completion, limiting the interpretation of our findings to sexually active populations.
It is expected that more people will utilize menstrual tracking applications given their ease of use, anonymity, and availability. Already, our study (41.6%) and other studies show a large percentage of the population obtains their primary reproductive health information from web/mobile-based applications47. Still, a limitation of utilizing study data from such applications is the reliance on self-reported data. As such, findings from the event logging data should be interpreted with caution, since participants were not specifically prompted to log this information but the study relied on existing logging data. These data are subject to participant logging behavior, which we attempted to account for by adjusting for non-sex-related event logging in our models. A further limitation is that we did not model associations between logged non-sex events, such as mood symptoms, and FSFI-6 scores, which may warrant further investigation. Our study also lacked data on factors that may affect sexual function, such as menopausal status, sexual partners, mental health, medication, and contraceptives, which are independent factors affecting sexual function. Lastly, our study was limited to people who menstruate. Future population-level investigations of sexual function should make increasing efforts to include individuals with diverse gender identities as sexual function in transgender and genderqueer populations continues to be understudied48.
Results of this study outline normative parameters for female sexual response and function in an ethnically and racially diverse reproductive age population of women in the United States. That sexual function may be compromised in women of underweight body habitus and in those with uterine fibroids can help guide individualized patient counseling and management. Since nearly half of participants cited web-based apps as their primary source of sexual health information, this study emphasizes the power of mobile/web-based apps in educating and advising patients on a population level. These methods may eventually be used to provide interventions for sexual health function.
Methods
Participants
Study participants were adult users of Flo in the United States. Eligible participants were sexually active in the four weeks preceding survey completion. Those who were pregnant or had given birth less than 6 weeks prior to the survey were excluded. Participants responded to a questionnaire via SurveyMonkey, provided by a link within the Flo app, between August 4 and September 4, 2023. Participants who did not complete the questionnaire were excluded from the analysis. A total of 5141 participants initially responded to the questionnaire, with the final study sample including 2392 respondents that met all of the inclusion criteria (Fig. 2).
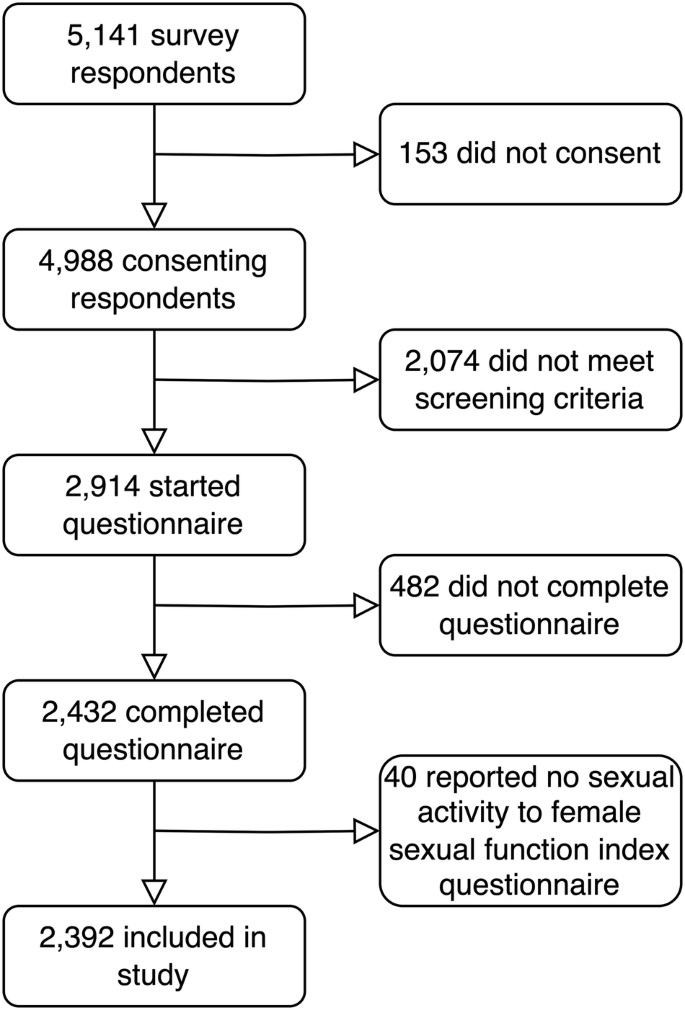
Study sample flow chart.
The mean age of respondents was 29.8 years (range: 18–54 years), with 54.0% self-identifying as White/Caucasian, 22.3% as Black or African American, and 14.4% as Hispanic (Table 2). A large proportion were parents (38.7%), had a higher education degree (42.9%), and used web/mobile apps as their primary source of sexual health knowledge (41.6%). A range of sexual orientations were represented, with 74.6% identifying as heterosexual or straight and 21.7% as bisexual. More than a quarter were trying to conceive (28.8%).
Materials
Participants self-reported sociodemographic information, including education, race, parity, and prior diagnoses of a selected list of health conditions that were focused on reproductive health. Sexual orientation, sexual activity, and main sources of sexual health knowledge, and a prior diagnosis and treatment of FSD were also queried. Finally, to characterize female sexual response, the questionnaire prompted participants to respond to the six statements from the FSFI-6 questionnaire regarding their sexual experiences in the four weeks before survey completion (Table 3)49. The FSFI-6 is shortened from the original 19-item FSFI to facilitate survey completion and assesses sexual function across six domains: desire, arousal, lubrication, orgasm, satisfaction, and pain. The FSFI-6 score was determined by totaling scores (between 1 and 5) for all six FSFI domains50. FSFI-6 scores could not be determined for participants who answered ‘No sexual activity’ to any of the FSFI-6 statements. Therefore, these participants were excluded from the study.
Design
Study participants provided electronic informed consent before completing the screening questions. Those who consented and met the inclusion and exclusion criteria (aged over 18 years, not pregnant or postpartum, report being sexually active in the preceding four weeks) could complete the survey on their mobile devices. We set out to survey approximately 5,000 respondents to account for an estimated attrition rate of 50% due to the strict inclusion and exclusion criteria.
A unique pseudonymized identifier was used to link survey responses to Flo application data for the respondents. Specifically, age, weight, height, and the primary purpose of app use (trying to conceive versus cycle tracking) at the time of survey completion were extracted. Self-reported weight and height data were used to compute body mass index (BMI) (underweight: BMI < 18.5 kg/m2; normal weight: BMI 18.5–24.9 kg/m2; overweight: BMI 25–29.9 kg/m2; obese: 30.0 kg/m2+).
Data from the in-app symptom, activities, and events tracking panel were also extracted retrospectively for the year preceding survey completion, meaning that study participants were not specifically prompted to log their symptoms for this study but the data were collected passively based on user logging. Logging data extracted for sexual activities and symptoms (referred to jointly as sex events throughout the remainder of this manuscript) included vaginal, oral, and anal sex, sensual touch, masturbation, use of sex toys, orgasm, and high and low sex drive. We also extracted logging of non-sex related events that include physical symptoms (pain, cramping, and digestive complaints, vaginal discharge), physical activity, and mood symptoms (angry, apathetic, confused, depressed, energetic, feeling guilty, happy, low energy, neutral, obsessive thoughts, panic, playful, sad, mood swings, very self-critical).
Ethics
The study was approved by the Independent Ethical Review Board: WIRB-Copernicus Group Institutional Review Board (IRB tracking number: 20233331). All research procedures were completed in accordance with the relevant ethical standards and guidelines of the Declaration of Helsinki. When choosing to participate in the study, participants consented to the use of their survey data and their Flo app data in aggregated and de-identified form for research purposes via our research informed consent form. This is in addition to the information provided to all users upon registration via our privacy policy, which states we may aggregate, anonymize, or de-identify their personal data and use it to contribute to the advancement of scientific research on female health. Study participants were not compensated for their participation.
Outcomes
The primary outcome of this study was sexual function as assessed by FSFI-6 score, with a higher score suggesting higher sexual function. Scores for individual FSFI domains (desire, arousal, lubrication, orgasm, satisfaction, and pain) were examined as secondary outcomes.
Statistical analysis
Statistical analyses included descriptive statistics of sociodemographic characteristics and female sexual function. Internal consistency of the FSFI-6 responses was assessed using Cronbach’s alpha. Using linear regressions, we estimated the associations between FSFI-6 scores and subdomain scores with 1) sociodemographic characteristics (age, education, race, parity, trying to conceive, sexual orientation, BMI, and primary sexual health knowledge source); 2) health conditions (ovarian cysts, polycystic ovary syndrome, sexually transmitted infection, thyroid disorder, endometriosis, and uterine fibroids) and 3) logging of sex events (vaginal, oral, and anal sex, logging high and low sex drive, masturbation, use of sex toys, orgasm, and sensual touch) in the Flo app.
Sexual event logging data were binarized as follows: we compared higher-than-average loggers of each sexual event to lower than or equal to average loggers. Higher-than-average loggers were defined as participants where the number of logs for respective sex events was above the population mean of logs for that event. Lower-than-average loggers were defined as the inverse, where the number of logs for the respective sex event was at or below the mean. To calculate the population mean for each sex event type, we took the total number of times each event was logged and divided it by the number of included users. We restricted these analyses to users who in addition to having logged sex events had also used the in-app symptom, activities, and events tracking panel to log other symptoms.
All linear regression models were multivariable models controlling for covariates that have previously been found to independently relate to our outcome measures of interest including age, education and trying to conceive, and health conditions queried27,28. The models for sexual event logging additionally adjusted for the number of non-sex-related logs to control for overall logging activity of each user. We generated 95% Wald confidence intervals and set statistical significance at p < 0.05. All analyses were completed in R version 4.3.051.

Responses