Grading the strength and certainty of the scientific evidence of the bidirectional association between periodontitis and noncommunicable diseases: an umbrella review

Introduction
Periodontitis is a chronic inflammatory disease primarily caused by a dysbiotic bacterial biofilm adhered to dental surfaces with the potential to exacerbate systemic inflammation, consequently leading to or worsening conditions such as cardiovascular diseases, diabetes, and respiratory diseases. The inflammatory mediators released during periodontal infections, such as cytokines and prostaglandins, can enter the bloodstream, contributing to systemic inflammation and promoting the development of systemic health complications [1, 2].
Noncommunicable diseases (NCDs) are medical conditions that cannot be transmitted directly from one person to another. They are usually chronic and progress slowly, frequently lasting for many years or even a lifetime. Cardiovascular complications, malignancies, chronic respiratory diseases, and diabetes are the four most common types of NCDs. These disorders are caused by a mix of genetic, physiological, environmental, and behavioral factors. Tobacco use, physical inactivity, a poor diet, and excessive alcohol consumption all contribute to metabolic alterations such as hypertension, obesity, hyperglycemia, and hyperlipidemia [3]. The impact of NCDs on human health is considerable, imposing a significant burden on individuals, healthcare systems, and economies around the world. NCDs are the main cause of mortality worldwide, accounting for over 74% of all deaths each year. They cause extended disability, lower quality of life, and higher healthcare costs. The chronic nature of NCDs involves long-term management and care, which places significant strain on healthcare resources. Furthermore, NCDs disproportionately impact low- and middle-income nations, where healthcare systems may be less suited to manage the complex and long-term care needed [3].
Periodontitis and some NCDs have a bidirectional relationship, meaning that the existence of one condition might influence the severity or progression of the other. This interaction is mostly explained by the systemic inflammatory response and immunological regulation. In 2016, Monsarrat and coworkers conducted a search related to periodontal medicine and reported that 57 systemic conditions have hypothetically associated with periodontitis. Apart from cardiovascular conditions, diabetes and adverse pregnancy outcomes which have abundant evidence, other diseases included anemia, liver diseases, dyspepsia and ankylosing spondylitis [4].
The complex relationship between periodontitis and NCDs emphasizes the significance of comprehensive healthcare treatments that address both oral and systemic health. Clinicians must acknowledge the interconnectivity of various NCDs and use a holistic approach to diagnose and treat the patients. For example, addressing periodontal disease may help manage systemic inflammation, positively impacting illnesses like cardiovascular disease and diabetes [5]. Likewise, effectively managing systemic conditions can contribute to better periodontal health, highlighting the need for collaborative care between dental and medical professionals. This integrated approach can lead to improved overall health outcomes and quality of life for patients.
The abundant publication of systematic reviews has resulted in an overwhelming collection of research that can be both repetitive and contradicting, which can cause scientific, ethical, economic, and social consequences [6]. While systematic reviews are useful for combining primary research, their methodology, quality, and scope can vary greatly, resulting in a range of results and recommendations. The large volume of these reviews can lead to information overload, making it challenging for physicians, policymakers, and academics to identify the most relevant and high-quality data needed for evidence-based decision-making.
Umbrella reviews address these challenges by providing a comprehensive synthesis of systematic reviews and meta-analyses on a particular topic. They offer a higher level of evidence by critically appraising and integrating findings from multiple systematic reviews, thus delivering a more cohesive and reliable summary of the existing research. Umbrella reviews enhance the clarity and utility of the evidence base, highlighting areas of consensus and identifying gaps or inconsistencies in the literature. Therefore, the purpose of this umbrella review is (1) to synthesize the evidence and (2) to grade the strength and certainty of the scientific evidence regarding the bidirectional association between periodontitis and NCDs.
Methods
An umbrella review was conducted according to the recommendations of the JBI (Joanna Briggs Institute) and adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) framework.
Focused question
Two focused questions were formulated using the PECO strategy depending on the direction of the association.
First direction: periodontitis is a risk factor for NCDs.
|
Population |
(P): |
adults. |
|
Exposure |
(E): |
periodontitis. |
|
Comparator |
(C): |
no periodontitis. |
|
Outcome |
(O): |
frequency of periodontitis in individuals with and without NCDs. |
What is the association between periodontitis and NCDs in adults?
Second direction: NCDs are a risk factor for periodontitis.
|
Population |
(P): |
adults. |
|
Exposure |
(E): |
NCDs. |
|
Comparator |
(C): |
no NCDs. |
|
Outcome |
(O): |
frequency of NCDs in individuals with and without periodontitis. |
What is the association between NCDs and periodontitis in adults?
Definition of NCDs
NCDs were defined as the most common systemic diseases that have been associated with periodontitis. To assist with the listing of possible NCDs, an artificial intelligence (AI-ChatGPT 4.0: searched July 24 2024) was used (see Supplementary Material 1). It is important to note that in some instances bidirectionality does not apply according to the current biological plausibility of the studied relationship and therefore was not included in the search.
Inclusion criteria
Only systematic reviews with meta-analysis were included in the review. There was no language restriction, but reviews published in languages other than Spanish or English were translated using an application.
Search strategy
A comprehensive search was conducted by two independent reviewers in MEDLINE (via PubMed), Embase and SciELO, restricted to a timeframe between January 2021 and July 2024, to retrieve the most recent evidence. The Cochrane Database of Systematic Reviews was not searched, as these reviews are included in PubMed and are typically limited to interventions. A list of keywords was used in various combinations (see Supplementary Material 2). The search was automatically restricted by time frame and type of article (i.e., systematic reviews).
Inclusion of systematic reviews
Initially, potential epidemiologic systematic reviews with meta-analysis that studied the bidirectional association between periodontitis and NCDs were identified by two independent reviewers and filtered by title and abstract according to the selection criteria. Subsequently, systematic reviews were selected for full-text review based on these criteria. Full-text articles were then retrieved, reviewed, and included. Any discrepancies between the reviewers were discussed, and if consensus could not be reached, a third reviewer made the final determination on study inclusion. The PRISMA flow diagram was used to illustrate the study selection process.
If multiple systematic reviews were identified for a given disease (e.g., diabetes), only the most recent report that met the inclusion criteria at the time of assessment was included to avoid overlapping. If the most recent systematic review did not meet the inclusion criteria, the next most recent review was considered, and so on. Critically low quality reviews were excluded as well as any other type of review that did not meet the inclusion criteria (e.g. animal studies, in vitro studies). Therefore, a single systematic review with meta-analysis was included for a singular disease depending on the availability of the evidence.
Data extraction
Data was extracted by two independent reviewers using a predetermined form that included: year and author, country of origin, systemic disease, number of studies, number of high risk of bias, number of events and totals in cases and comparator, odds ratio/risk ratio/hazard ratio with 95% confidence intervals, I2, Chi2 (with p value) and publication bias.
Quality assessment of systematic reviews
The quality of the systematic review was classified by two independent reviewers (high 8–11, moderate 4–7, low 0–3) according to the JBI critical appraisal checklist for systematic reviews and research. Although the checklist is not intended as a quantitative tool, it allows to identify potential issues in the design of the systematic reviews that may affect the quality of the results. Any discrepancies between the reviewers were discussed, and if consensus could not be reached, a third reviewer made the final determination on study quality.
Grading the strength and certainty of the evidence
An initial grading of the strength of the association was based on the assessment of the size of the reported effect (odds/risk ratio) according to Rosenberg and Handler [7]. The classification was as follows: none (1.0–1.2), weak (1.2–1.5), moderate (1.5–3.0), and strong (3.0–10.0).
The quality and certainty of the evidence was assessed according to the Grading of Recommendations, Assessment, Development and Evaluations (GRADE) guide. If the systematic review did not include a GRADE assessment, one was performed based on the published data.
Synthesis of effect measurement
All study data were tabulated and presented in the qualitative synthesis. The effect measurement was the reported odds ratio (OR)/relative risk (RR)/hazard ratio (HR) with its 95% confidence interval for each NCD. The Chi² test was used to determine heterogeneity among the included studies, and the I² statistic was applied to estimate its impact. The I² value was categorized as follows: 0–40% indicating mild heterogeneity; 30–60% indicating moderate heterogeneity; 50–90% indicating substantial heterogeneity; and 75–100% indicating very considerable heterogeneity.
The measurements of effect size were plotted according to the strength of the association for each systematic review and NCD.
Results
General characteristics of the systematic reviews
Initially, 561,554 potential results were identified. After removing duplicates and excluding records deemed ineligible by automated filters, 450 results were screened by title and abstract. This process led to 41 records being appraised in full-text. Of these, 17 were further excluded (see supplementary material 3), leaving a total of 24 systematic reviews [8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31] that met the inclusion criteria (Fig. 1).
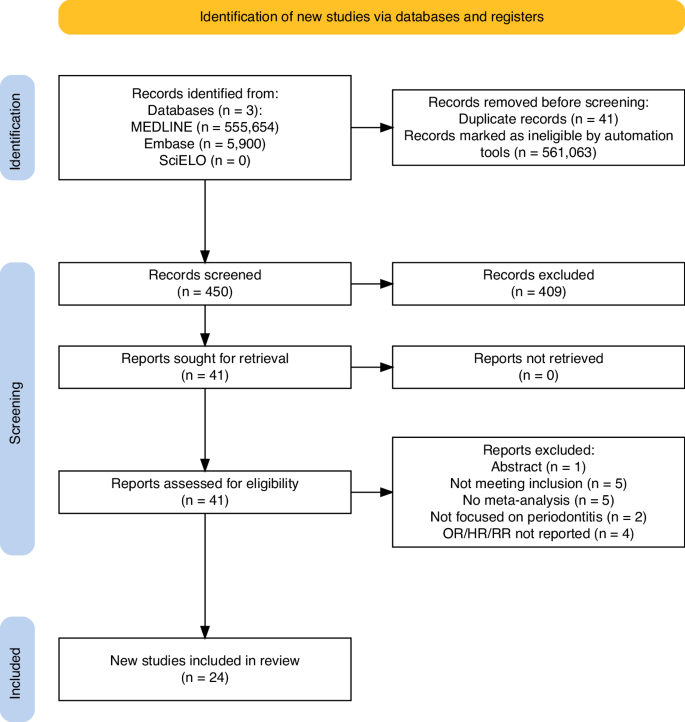
Flow diagram of systematic reviews selection.
Table 1 lists the general characteristics of the included systematic reviews. In total, 32 NCDs were studied and consolidated: pregnancy complications (preterm birth, low birth weight, preeclampsia), cognitive impairment, cardiovascular complications (heart failure, stroke, myocardial infarction, coronary heart disease, atrial fibrillation, atrial flutter), cancers (oral, lung, colorectal, urogenital, gastric, pancreatic), gastrointestinal disease (inflammatory bowel disease, Crohn’s disease, ulcerative colitis), Sjogren’s syndrome, sleep disordered breathing, obesity, dyslipidemia, diabetes, hyperglycaemia, liver disease, osteoporosis, rheumatoid arthritis, chronic obstructive pulmonary disease, metabolic syndrome, systemic lupus erythematosus and kidney disease. In general, the majority of the systematic reviews were registered and publication lag time was 1 year on average. The methods of determining the diagnosis of the NCDs and periodontitis varied among studies but in general used clinical examination, the International Classification of Diseases codes, well established criteria, national records and self-reporting. The number of included studies in the systematic reviews ranged from 3 to 33 and publication bias was evident.
The risk of bias assessment indicated that 21 systematic reviews (87.5%) demonstrated low bias (high quality) [8,9,10,11,12,13, 15,16,17,18,19, 21,22,23,24,25,26,27, 29,30,31], 2 had medium bias [14, 28], and 1 exhibited high bias (low quality) [20]. Key issues identified included the formulation of explicit research questions, critical appraisal, data extraction, and publication bias (Fig. 2 and Supplementary Material 4). Two systematic reviews with meta analysis were published in the format of rapid communication and therefore lacked some information in the methods [14, 20]. However, they were kept since they analyzed the influence of periodontitis on two cardiovascular conditions that were not identified in other reviews.
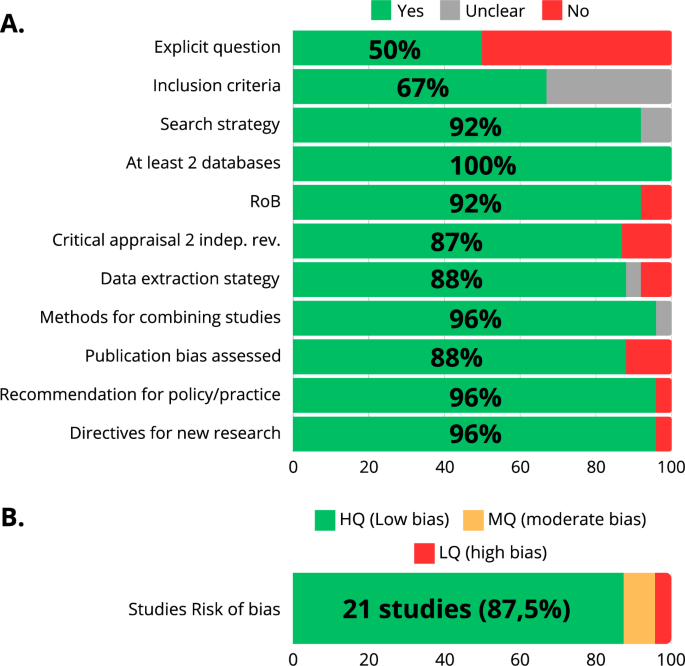
A Shows the frequency distribution of the quality domains. B Shows the general risk of bias of the systematic reviews.
The association between periodontitis and NCDs
The strength of the association between periodontitis and NCDs is presented in Fig. 3. The estimate of the association was strong in 1 systematic review (preeclampsia), moderate in 8 (oral cancer, low birth weight, metabolic syndrome, kidney disease, preterm birth, cognitive impairment, heart failure, liver disease), weak in 10 (colorectal cancer, lung cancer, osteoporosis, pancreatic cancer, atrial fibrillation and flutter, stroke, rheumatoid arthritis, urogenital cancer, diabetes, cardiovascular complications in men), and absent in 7 systematic reviews (chronic obstructive pulmonary disease, gastric adenocarcinoma, dyslipidemia, ulcerative colitis, cardiovascular complications in women, inflammatory bowel disease, Crohn’s disease). The size of the reported effect was broader with increasing strength and this should be interpreted cautiously. Periodontitis significantly increases the odds of preeclampsia (OR 3.18; 95% CI 2.26–4.48), with the confidence interval not including 1, though it appears somewhat wide. This suggests that there is substantial evidence supporting an association between periodontitis and preeclampsia. Conversely, the relative risk (RR) of liver disease is 1.53 (95% CI 0.86–2.73), with a confidence interval that includes 1 and is wide, indicating a moderate but unstable association between periodontitis and liver disease. Finally, the odds ratio for stroke, myocardial infarction, and coronary heart disease in women is 1.11 (95% CI 1.05–1.17), which does not support an association between periodontitis and these cardiovascular events.
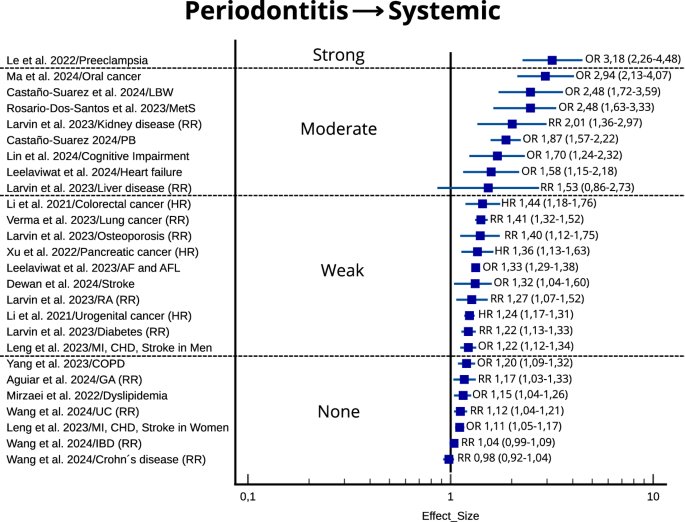
OR odds ratio, HR hazard ratio. 95% confidence interval is shown in parenthesis. LBW low birth weight, MetS metabolic syndrome, PB preterm birth, AF atrial fibrillation, AFL atrial flutter, RA rheumatoid arthritis, MI myocardial infarction, CHD coronary heart disease, COPD chronic obstructive pulmonary disease, GA gastric adenocarcinoma, UC ulcerative colitis, IBD inflammatory bowel disease.
The association between NCDs and periodontitis
The strength of the association between NCDs and periodontitis is depicted in Fig. 4. The estimate of the association was moderate in 6 systematic reviews (systemic lupus erythematosus, Sjogren’s syndrome, Crohn’s disease, sleep disordered breathing, rheumatoid arthritis, type 2 diabetes) and weak in 3 systematic reviews (hyperglycaemia, inflammatory bowel disease, obesity). In general, the reported size of the effect was broader also with increasing strength, which as result impacted the precision of the certainty of the evidence. In summary, the evidence suggests that certain NCDs are associated with periodontitis, but the wider confidence intervals indicate that these findings should be interpreted with caution.
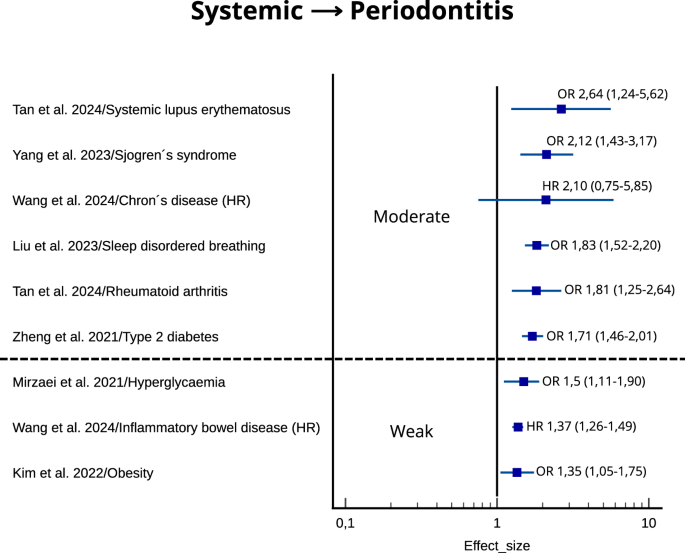
OR odds ratio, HR hazard ratio. 95% confidence interval is shown in parenthesis.
Certainty of the evidence for the bidirectional association between periodontitis and NCDs
Although data supports the association between periodontitis and NCDs, and to a lesser extent between some NCDs and periodontitis, the certainty of the evidence was classified as low to very low (Tables 2 and 3). This means that our confidence in the effect estimates is very limited and the actual effect is likely to be substantially different from the effect estimate. It is important to note that the level of certainty was primarily downgraded due to potential risks of bias, as well as heterogeneity in both the effect sizes and study methodologies, which impacted the precision of the results.
Discussion
The results of this umbrella review objectively compile the best available evidence regarding the bidirectional association between periodontitis and systemic health. However, even the highest quality evidence may not always be sufficient to draw definitive conclusions that inform clinical decision-making. To date, aside from the review by Botelho et al. [32], this study is the most recent and specifically addresses the grading of evidence certainty in this area. In addition, it does not focus on biological mechanisms but rather examines data derived from various analytical studies in humans.
Significance of the results
Is periodontitis a risk factor for systemic health complications and vice versa, or is it merely coincidental? The results of this umbrella review indicate that while periodontitis is associated with certain NCDs, it does not establish a causal relationship. The most plausible explanation is that periodontitis and systemic health issues often occur simultaneously and share common inflammatory and microbiological mechanisms. Consequently, the presence of one condition may influence the development of the other. The studies included in this review highlighted the co-occurrence of multiple systemic conditions and confounding factors. Therefore, it is not possible to confirm that periodontitis independently contributes to systemic health complications and vice versa.
Multimorbidity is the presence of two or more chronic conditions in an individual, with no one ailment being regarded as the dominant focus. This phenomenon is becoming more common in aging populations and poses considerable challenges to healthcare systems because of the complexities of addressing many, often interconnected, diseases at the same time. Multimorbidity complicates clinical decision-making while also increasing the strain on patients, who must navigate many therapies and healthcare providers. It is linked to higher healthcare expenses, lower quality of life, and increased mortality, emphasizing the importance of integrated and patient-centered approaches to care. Large population-based studies have demonstrated that a significant proportion of adults—27%—report having two or more chronic conditions, with the prevalence increasing notably with advancing age [33, 34]. In our umbrella review, periodontitis appears to be associated with some systemic chronic diseases (i.e. systemic lupus erythematosus to periodontitis or periodontitis to preeclampsia) and tend to co-occur, primarily because they share common inflammatory mechanisms, as well as genetic, environmental, and sociodemographic determinants. Therefore, periodontitis remains a significant condition in the context of multimorbidity because it has the ability to contribute to and be affected by several chronic diseases. Understanding the link between periodontitis and multimorbidity is critical for establishing holistic care methods that target the underlying causes of these non-communicable chronic diseases to reduce the health impact of aging.
Limitations of this review and perspective
The main limitation of this umbrella review is that the quality of the evidence is inherently influenced by the quality of the original research. Inconsistencies and contradictions among the included studies can complicate the interpretation of the overall findings. Each systematic review identified potential sources of bias, which must be considered when evaluating the results. Consequently, the certainty of the evidence was rated as low. This suggests that the conclusions drawn from the studies should be approached with caution, given the challenges associated with investigating the interactions between periodontitis and systemic conditions in humans.
To enhance the quality of data supporting the link between periodontitis and NCDs, future research should focus on well-designed longitudinal studies that minimize bias and appropriately consider multimorbidity. This involves utilizing statistical models that account for the effects of multiple chronic diseases, as well as employing standardized diagnostic tools. Additionally, to address health disparities and improve overall population health, it is essential to understand how socioeconomic, racial, and ethnic factors influence the prevalence, severity, and accessibility of treatment for both systemic diseases and periodontitis.
Conclusions
There is some data that, with varying degrees of association and low to very low certainty, provide evidence that periodontitis may be a potential risk factor for some NCDs and vice versa.



Responses