Investigating racial disparities in drug prescriptions for patients with endometriosis

Introduction
Endometriosis is a chronic, inflammatory disease characterized by growth of endometrial-like tissue outside the uterus. Identified symptoms of endometriosis vary widely and include dysmenorrhea, fatigue, non-menstrual abdominopelvic pain, and heavy menstrual bleeding1,2. While the precise prevalence of endometriosis is unknown, it affects an estimated 6–10% of women of reproductive age2,3,4. Current medical interventions for endometriosis depend on patient prognosis and include analgesics, combined hormonal contraceptives, progestogens, gonadotropin-releasing hormone (GnRH) agonists, GnRH antagonists, aromatase inhibitors, and surgical treatments5.
Racial health disparities in the United States are pervasive, and research shows that Black and Hispanic patients are less likely to receive a diagnosis of endometriosis compared to White patients6, as well as less likely to receive surgical treatment for endometriosis7. Racial bias is observed beyond endometriosis diagnosis, such as in pain management; Black and Hispanic patients are less likely to be treated for pain and other symptoms that impact quality of life8,9,10,11.
In this work we characterize the drug prescription patterns for endometriosis patients and potential differences in prevalence across Black and White patients. First, we take a data-driven approach to identify a broad range of medications associated with treatment of endometriosis and comorbidities; this allows us to identify medications that may not be present in the clinical guidelines but are used to address side effects or comorbidities across various body systems. We then introduce a temporal dimension to our analysis: due to the long lag to diagnosis, suspected endometriosis patients may be prescribed relevant treatments prior to their official diagnosis. We do this by comparing patterns in prescriptions across Black and White endometriosis patients prior to their diagnosis, after diagnosis, and overall. We use propensity score matching to adjust for age at endometriosis diagnosis, duration of observation window prior to diagnosis, and duration of observation window after diagnosis. Finally, we further contextualize our analysis by comparing the race-based differences we observe in the endometriosis cohort to those in a non-endometriosis comparison cohort, thus allowing us to identify differences that are specific to or heightened amongst endometriosis patients.
Results
Cohorts and medications
The non-endometriosis cohort comprises 3,663,904 patients (Table 1). The endometriosis cohort (n = 16,372) comprised more White patients (66%) than the non-endometriosis cohort (50%). The endometriosis cohort was slightly older (mean age 32.4 ± 8.0 years) than the non-endometriosis cohort (28.7 ± 10.3 years). The median length of observational period was 6.08 (IQR: 5.08–8.84) years for the endometriosis cohort and 4.00 (IQR: 2.00–6.25) years for the non-endometriosis cohort. For the endometriosis cohort, the median length of observation prior to diagnosis was 4.20 (IQR: 3.26–5.73) years, and the median length of observation post-diagnosis was 1.68 (IQR: 0.82–2.89) years.
Prior to propensity score matching, Black patients are significantly older than White patients (34.0 vs. 31.8 years, p-value = 1.7e−45) and they have significantly more time within their observation periods both pre- and post-diagnosis (pre-diagnosis: 5.4 vs. 4.9 years, p-value = 5.8e−38; post-diagnosis: 2.8 vs. 2.5 years, p-value = 2.5e−16). Within the matched population, none of these mean values are significantly different (age: 34.0 vs. 33.7 years, p-value = 0.20; pre-diagnosis observation time: 5.4 vs. 5.3 years, p-value = 0.63; post-diagnosis observation time: 2.8 vs. 2.9 years, p-value = 0.15).
Overview of hormonal drug classes
To gain more clarity about the differences in hormonal prescriptions, we investigate the specific drugs and overlap between the four drug classes: estrogens, progestogens, hormonal contraceptives for systemic use, and hormones and related agents. Estrogens includes oral, injectable, transdermal, topical, and vaginal (vaginal cream, vaginal system, and vaginal insert) preparations. Progestogens includes oral, injectable, and vaginal (vaginal gel, vaginal suppository) preparations. Hormonal contraceptives for systemic use include oral tablets, injectables, and drug implants; notably, hormonal intrauterine devices belong to a separate category, contraceptives for topical use that was not included because the prevalence did not differ significantly between the endometriosis and non-endometriosis cohorts. Hormones and related agents included oral, injectable, and implanted medications. Names of specific drugs belonging to each of these classes can be found in Supplementary Table 1.
Many drugs belong to multiple ATC Level 3 classifications, particularly if they have multiple active ingredients. For example, conjugated estrogens and medroxyprogesterone belongs to estrogens, progestogens, and hormones and related agents. Estradiol-based contraceptives belong to both estrogens and hormonal contraceptives for systemic use. Medroxyprogesterone, medroxyprogesterone acetate, and megestrol acetate belong to progestogens, hormonal contraceptives for systemic use, and hormones and related agents. We also observe several GnRH agonists categorized within hormones and related agents (e.g. leuprolide, histrelin, goserelin).
Differences in overall prevalence of drug prescriptions for Black and White patients
Of the 28 drug classes of interest, 17 (61%) are prescribed significantly more often for White endometriosis patients and 4 (14%) were prescribed significantly more often for Black endometriosis patients (Fig. 1). In the non-endometriosis cohort, 21 (75%) are prescribed significantly more for White patients and 6 (21%) are prescribed significantly more for Black patients.
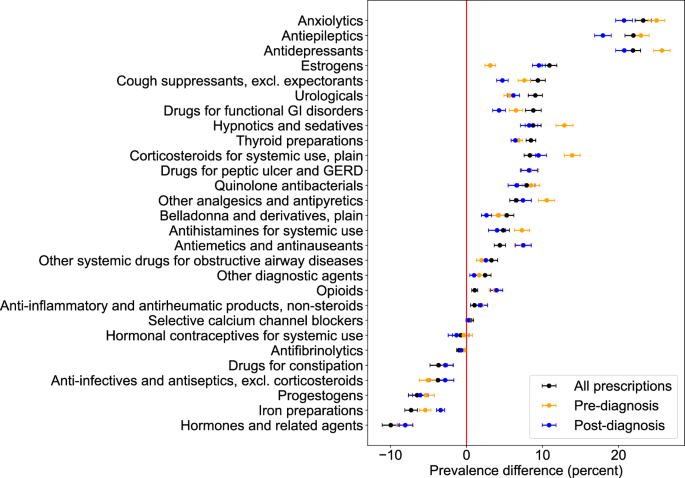
This graph shows the percent difference in drug class prescription prevalence between White and Black patients. Error bars indicate standard error, and a difference greater than 0 indicates that White patients are prescribed a drug from that class with higher prevalence than Black patients. The percent difference is shown across all visits, visits prior to diagnosis (subgroup 1), and visits after diagnosis (subgroup 2).
The largest racial differences in endometriosis patients occur for anxiolytics (prescription prevalence higher by 23.2% in White patients than Black patients, 95% CI [21.2%, 25.3%]), antiepileptics (22.0%, 95% CI [19.8%, 24.1%]), antidepressants (21.9, 95% CI [19.9%, 23.9%]), and estrogens (10.9%, 95% CI [9.0%, 12.8%]). For drug classes where Black patients are prescribed with higher prevalence then White patients, the largest differences occur for hormones and related agents (10.0%, 95% CI [7.7%, 12.2%]), iron preparations (7.3%, 95% CI [5.7%, 8.9%]), and progestogens (6.5%, 95% CI [4.3%, 8.7%]). Prescription prevalence differences are more pronounced in the endometriosis cohort than the non-endometriosis cohort for anxiolytics, antiepileptics, estrogens, iron preparations, and hormones and related agents but are less pronounced in the endometriosis cohort for antidepressants and progestogens (Table 2).
Out of the drug classes related to established endometriosis treatment options, one (other analgesics and antipyretics) is significantly more prevalent amongst White endometriosis patients and two (hormones and related agents, progestogens) are significantly more prevalent amongst Black endometriosis patients (Table 2). These differences are generally consistent with the non-endometriosis cohort.
Temporal differences in drug prescription disparities
When observing drug prescription differences across White and Black endometriosis patients across temporal subgroups, there is a pattern of pre-diagnosis differences (temporal subgroup 1) exceeding post-diagnosis differences (temporal subgroup 2), especially for drug classes where White patients are prescribed at a higher rate (Fig. 1 and Table 3). Of the 17 drug classes that fall into this category, 13 (76%) have larger differences prior to diagnosis compared to post-diagnosis. For drugs that are significantly more prevalently prescribed in Black patients, 1 (25%) has a higher prevalence difference pre-diagnosis than post-diagnosis.
Discussion
Our analysis of drug prescription patterns amongst White and Black patients with endometriosis shows that broad racial differences in disease treatment and pain management exist within endometriosis. We find that disparities in prescription prevalence are larger prior to endometriosis diagnosis (compared to after the endometriosis diagnosis). Given previously observed racial disparities in endometriosis diagnosis6, it becomes especially important to study this pre-diagnosis period, where the patient may require treatment but has no formal diagnosis to explain the multi-system, chronic symptoms they may be facing. We additionally find that drugs associated with comorbidities of endometriosis (including gastrointestinal distress, irritable bowel syndrome, thyroid disorders, and lower urinary tract symptoms12,13,14) are prescribed significantly less prevalently in Black patients; this suggests disparities in holistic endometriosis management that are not fully explained by general disparities in access to prescription medications.
The most notable differences in prescription prevalence occur for antidepressants and anxiolytics. Notably, the difference in anxiolytic prescription prevalence is larger amongst endometriosis patients than non-endometriosis patients. Prior studies have noted disparities in the prescription of antidepressants15,16 and select anxiolytics17, with literature suggesting that this may be due to Black patients experiencing less rapport-building during visits18 and being less likely to communicate symptoms to healthcare providers18,19. This gap in physician-patient communication could be due to a lack of cultural competency and/or perceived racism20,21, both of which contribute to healthcare-related stress22,23,24. Future qualitative work should investigate how healthcare-related stress manifests differently for endometriosis patients based on race, particularly those with comorbid mental health conditions.
We additionally observe that Black patients are less likely to receive pain medications (both opioid and non-opioid) than White patients. This disparity is similar for endometriosis and non-endometriosis patients and is consistent with the literature8,9,10,11. However, the temporal analysis shows that the disparity is larger for endometriosis patients pre-diagnosis compared to post-diagnosis; furthermore, the disparity in non-opioid analgesic prescriptions is larger in the pre-diagnosis endometriosis cohort than the general comparison cohort. Prior to diagnosis, patients may experience pain-related symptoms without an explicit diagnosis of endometriosis to explain that pain; our results suggest that at this point, racial disparities are heightened beyond those that exist in the general population.
There are several factors that impact systemic inequities related to pain medication prescription, including false stereotypes about Black patients exhibiting “drug-seeking behavior”25,26 or feeling less pain than their White counterparts8. Additionally, racism experienced by Black patients when seeking chronic pain treatment may contribute to hopelessness (negative expectations about one’s present life and future), which can negatively impact pain management10. Lack of effective communication between patients and physicians surrounding medication tolerance, side effects, efficacy, and addiction has also been found to disproportionately impact racial and ethnic minorities24. Further work is required to understand how people with undiagnosed chronic disease (i.e. endometriosis) experience pain management and how this differs from the general population.
Our use of the Multi-state Medicaid Dataset enables us to create a large cohort of endometriosis patients with consistent access to care. Given that Medicaid users are also predominantly part of low-income households, ensuring racial equity in treatment for Medicaid users is critical to fighting the systemic and intersectional health disparities that persist in the United States27. Due to the wide variety of healthcare settings represented within the multi-state Medicaid dataset, we believe our findings will be generalizable across insured populations within the United States. The large size of the Medicaid database also allows us to take a data-driven approach to identify medications, which is especially important when considering the holistic care of a chronic and multi-system disease like endometriosis2.
However, our approach does have limitations. While we adjusted for temporal confounders (age and duration of observation), we were unable to adjust for sociodemographic variables. Our use of the Medicaid dataset implicitly controls for income, as Medicaid predominantly serves low-income individuals, but we do not have access to more fine-grained economic information, education, location, or other community contexts. We are also unable to adjust for parity, drug contraindications, or other variables related to a person’s medical history, as we do not have access to information about a patient outside of the years they are in the dataset. Future work should focus on better understanding the context surrounding drug prescription patterns and could leverage comorbid conditions and self-reported data to provide more information about why a drug is prescribed.
Our work is limited in its generalizability to uninsured populations within the United States and to international populations, where medical inequities may differ from those in the United States. Due to limitations of the recorded data, we were also unable to study differences across ethnicity or race categories other than Black and White. Additionally, we use a validated phenotype28 to define our endometriosis cohort and we define the “date of diagnosis” as the date of laparoscopic surgery; while this definition does ensure a highly specific cohort, it is not fully aligned with current clinical guidelines, which recommend that treatment be explored if imaging tests indicate endometriosis5. Some prescriptions occurring in the “pre-diagnostic” period therefore may be treating endometriosis confirmed through imaging. This phenotype also uses a “female” gender marker as inclusion criteria, which may exclude some transgender men with endometriosis. The use of ATC level 3 drug classes enables us to quickly and accurately pull relevant drugs based on their pharmacological functions while remaining robust to differing prescription patterns across states29,30; however, ATC medication classes are intended to reflect the drug indication, which may not always be consistent with why the drug was prescribed.
In this work, we document racial disparities in medication prescription practices for Black endometriosis patients; these disparities exist in several aspects of treatment and are reflective of Black patients not receiving holistic endometriosis care. We compare these disparities to a non-endometriosis population and find several drug classes where disparities are larger in the endometriosis population, indicating that these disparities are unique to chronic disease management (and potentially to endometriosis). When coupled with the fact that these prescription disparities are larger pre-diagnosis compared to post-diagnosis, it becomes important for clinicians who treat chronic, complex patients to ensure that they are communicating with their patients and prescribing medications consistently and equitably.
Methods
The analysis and the use of the de-identified dataset presented in this work were carried out under Research Protocol AAAO7805 approved by Columbia University Institutional Review Board. All ethical regulations were followed, including the Declaration of Helsinki. Informed consent was waived by the IRB due to low risk to subject welfare and logistical infeasibility of contacting millions of patients from a de-identified database.
Dataset
In this retrospective cohort study, we focus our analysis to patients with Medicaid, a U.S. government program that provides health insurance for people with limited income. The data comes from the Merative MarketScan® Multi-state Medicaid dataset, which draws Medicaid data from several states (https://www.merative.com/documents/brief/marketscan-explainer-general). The Medicaid dataset contains de-identified longitudinal records of patients between 2008 and 2017 and includes inpatient and outpatient services, diagnostic history, and drug prescriptions for over 25 million enrollees. We leverage the data under the OMOP Common Data Model (CDM) format, which follows standardized conventions for drugs, therapies, and other medical vocabularies31. The database has been used for a variety of observational health studies due to its flexibility and robustness32,33.
Cohort identification
We select patients with endometriosis using a validated cohort definition28. The cohort definition includes all women ages 15–49 years who have an endometriosis-related surgical procedure (e.g., laparoscopic surgery) and a diagnosis of endometriosis within 30 days of this procedure. The phenotype definition was validated through manual chart review of 1400 endometriosis patients and reported to achieve 70% sensitivity, 93% specificity, 85% positive predictive value. Age is calculated based on the date of the surgical procedure. Patients with endometriosis must have at least three years of continuous observation prior to diagnosis.
The non-endometriosis cohort comprises of any female aged 15–49 with no diagnostic codes for endometriosis and at least one year of continuous observation. Age is calculated using the most recent visit date.
Identification of medications
The Anatomical Therapeutic Chemical (ATC) classification system separates drugs based on their functions and the chemical properties of their active ingredient. For this study, we use ATC level 3 classifications because they are associated with specific pharmacological functions without specifying chemical structures (https://www.who.int/tools/atc-ddd-toolkit/atc-classification). We use the OMOP Common Data Model to explicitly map medications to their ATC level 3 classification, with the ATC classifications serving as a “bridge” between the clinical guidelines for endometriosis and large-scale observational health data.
We narrow the set of drug classes by identifying drug classes that are prescribed significantly more often in the endometriosis cohort than the non-endometriosis one. For each drug class, the proportion of patients in each cohort with at least one prescription belonging to that drug class is calculated. The statistical significance of the difference between these relative prevalence measurements is calculated using a two-sided Z-test with a 0.01 significance level. This procedure identified 28 drug classes that are significantly more prevalent in the endometriosis cohort than the non-endometriosis cohort (Supplementary Table 2); we then measure prescription prevalence for each of these drug classes. Supplementary Table 1 lists the most common medications per drug class in the endometriosis cohort and non-endometriosis cohort.
To understand the clinical relevance of these 28 drug classes, we checked them against the drugs listed in the 2022 ESHRE guidelines for treating endometriosis5. The only recommended treatments that are not included in our analysis are GnRH antagonists and aromatase inhibitors. GnRH antagonists were not prescribed in the Medicaid dataset, and aromatase inhibitors were excluded because the corresponding ATC 3rd level drug class (“hormone antagonists and related agents”) was not prescribed significantly more in patients with endometriosis than in the non-endometriosis cohort. This data-driven approach identified several additional drug classes more prevalently prescribed in the endometriosis population that are associated with known comorbidities or symptoms of endometriosis including gastrointestinal distress, depression, and anxiety34,35.
Temporal analysis
Endometriosis is known to have extended delays between symptom onset and diagnosis36,37. We therefore aim to better understand the patterns of drug prescription prior to diagnosis (which occurs via laparoscopic surgery) and whether they differ from prescription practices after diagnosis. Prescription practices from the pre-diagnosis period can be thought of as prescription practices for undiagnosed endometriosis patients, which is an important area of study given that Black patients are less likely to be diagnosed with endometriosis compared to White patients6.
We create two temporal subgroups of drug prescriptions in the endometriosis cohort (Fig. 2). Subgroup 1 consists of all prescriptions occurred prior to surgical diagnosis. Subgroup 2 consists of all prescriptions post-diagnosis. Note that neither subgroup contain prescriptions from the day of diagnosis; these prescriptions are only counted in the “overall” prescriptions.
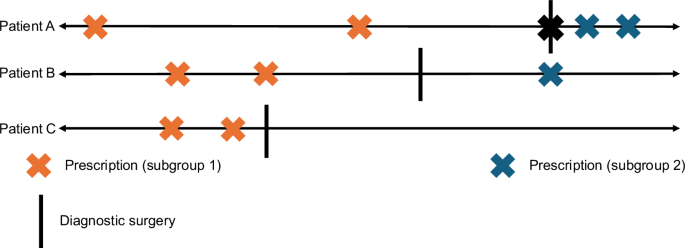
Three example longitudinal records are shown, with prescriptions marked as “x” and a laparoscopic diagnosis of endometriosis marked with a vertical line. As shown in the figure, prescriptions ordered prior to diagnosis fall into subgroup 1 (pre-diagnosis, orange) and prescriptions ordered after diagnosis fall into subgroup 2 (post-diagnosis, blue). Prescriptions from the day of diagnosis are not counted in either subgroup.
Statistical methods
We use propensity score matching to control for confounding in the endometriosis cohort based on three temporal variables: age at endometriosis diagnosis, amount of observation time prior to diagnosis, and amount of observation time after diagnosis. Observation periods were determined based on the patient’s earliest available observation start date and latest available observation end date, respectively. We use the procedure outlined in Garrido et al.38 to implement propensity score matching and checked population differences before and after matching using t-tests. We select matches based on nearest-neighbors and perform 1:1 matching without replacement39. We do not adjust for these variables in the non-endometriosis cohort, as there is no equivalent “diagnosis date” for non-endometriosis patients.
For each drug class of interest, the relative prevalence of prescriptions within that drug class was calculated for Black and White endometriosis patients. A person is counted as part of the drug-positive group if they received at least one prescription from that drug class, and prevalence is calculated relative to the total number of Black and White patients in the endometriosis cohort, respectively. The difference in prescription prevalence is calculated as (100 % * {(p}_{{white}}-{p}_{{black}})), where ({p}_{{white}}) and ({p}_{{black}}) are the fraction of patients who received at least one drug within that drug class out of all of the patients of that race (Tables 2 and 3).
To identify significant differences in the Black and White sub-populations, we conduct a two-sided Z-test from the difference in prevalence and the associated standard error. We apply the Bonferroni correction to account for multiple comparisons; we consider the difference significant when the adjusted p-value < 0.01. This procedure for statistical analysis was repeated for all prescription classes and both temporal subgroups (pre-diagnosis and post-diagnosis). Analysis was carried out using the scipy package in Python40.




Responses