Tackling antibiotic resistance—insights from eHealthResp’s educational interventions

Introduction
Antibiotic resistance (AR) represents a major global public health challenge1. The misuse and overuse of antibiotics, as well as the natural process of bacterial evolution, have resulted in the emergence of antibiotic-resistant bacterial strains, making it increasingly difficult to treat infectious diseases, namely respiratory infections2,3,4.
AR can affect anyone and is a growing problem in both developed and developing countries5. In addition to therapy failures, other problems are involved, such as an increased rate of infections and their severity, increased health costs and longer hospital stays, and global spread of antibiotic-resistant strains, having a significant, negative, impact on vulnerable populations6,7. Furthermore, it leads to microbial interactions which contributes to a modified environment of microbial communities8. Moreover, the development of new antibiotics has not kept pace with the emergence of antibiotic-resistant bacteria, resulting in a limited range of treatment options9. Therefore, it is crucial to raise awareness among healthcare professionals to improve prescription practices and the daily use of antibiotics to avoid exacerbating AR in the community10,11.
Currently, studies suggest that this public health problem could be reduced by promoting educational interventions focusing on healthcare professionals, ensuring wide-ranging and informed knowledge before prescribing antibiotics to patients12,13,14. Furthermore, education about this topic could lead to a reduction in the misuse and unnecessary consumption of antibiotics for the treatment of certain respiratory tract infections14,15,16,17,18, and possibly slowing down the growing levels of AR, currently causing 33,000 yearly deaths in Europe15. Therefore, promoting literacy on this topic has several advantages for the community, consequently preserving and minimizing the use of new antibiotics as much as possible, aiming for a future where these antibiotics can be employed without the concern of microbial agents developing resistance19,20.
Health literacy on AR, comprising antibiotic consumption and appropriateness of prescription topics, can be achieved through digital health tools, which have been increasingly useful in addressing healthcare professionals’ education21,22,23. The use of digital health tools among healthcare professionals presents a promising solution to overcome some health workforce-related challenges by offering enhanced accessibility, relevance, standardization, timeliness, and affordability of medical education and training23,24. Consequently, they can act as clinical supporting tools aiming to improve clinical decision-making, allowing a reduction in medication errors and better patient monitoring21,25,26,27. Technological development and new information make these digital health tools more relevant in clinical decision-making, contributing to the improvement of antibiotic prescribing, and to update the information used by healthcare professionals in the field of AR28,29,30.
In this way, eHealthResp was created, a clinical decision support tool related to upper respiratory tract infections (URTIs), including an online course and a mobile application aimed at primary care physicians and community pharmacists, supporting adequate antibiotic use12,31,32,33,34. Therefore, the main goal of this study is to analyse the usage patterns of the eHealthResp online course and the mobile app by primary care physicians and community pharmacists.
Results
Pharmacists’ eHealthResp online course
The eHealthResp online course was explored by 17 pharmacists, although a total of 44 pharmacists attended the educational intervention. Figure 1 illustrates the enrollment of pharmacists in the eHealthResp online course.
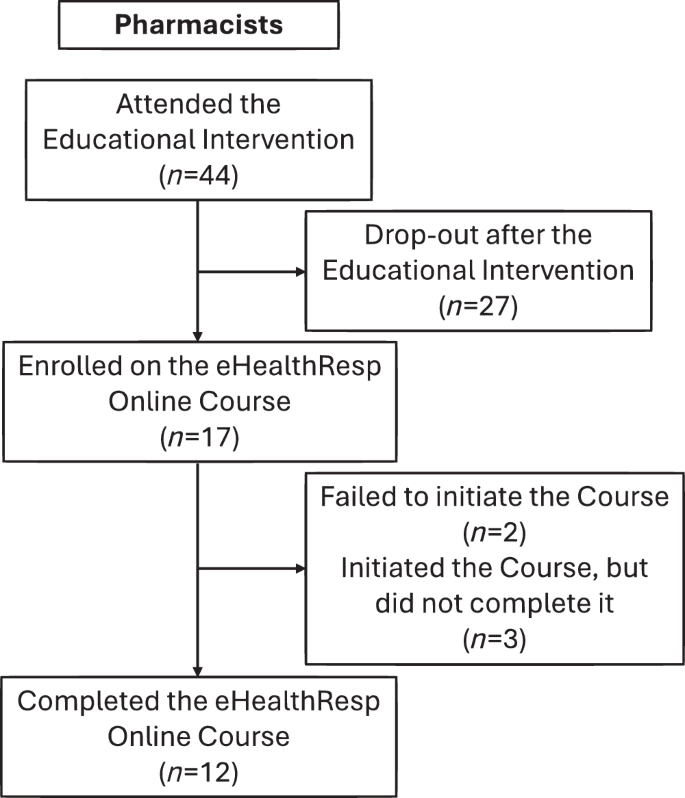
The flowchart outlines the recruitment process and course participation steps of the 44 pharmacists, with 17 completing the online course.
Among these participants, the average progress rate was 74%, with 5 pharmacists not completing the course. This indicates that while these participants initially registered for the course and started it, they did not complete all the modules. Of those 5 pharmacists, 2 made no progress in the online course, indicating that they failed to initiate it. All the 12 pharmacists that completed the online course achieved a grade of 100%.
Figure 2 presents the eHealthResp online course progress rate for this group of healthcare professionals.
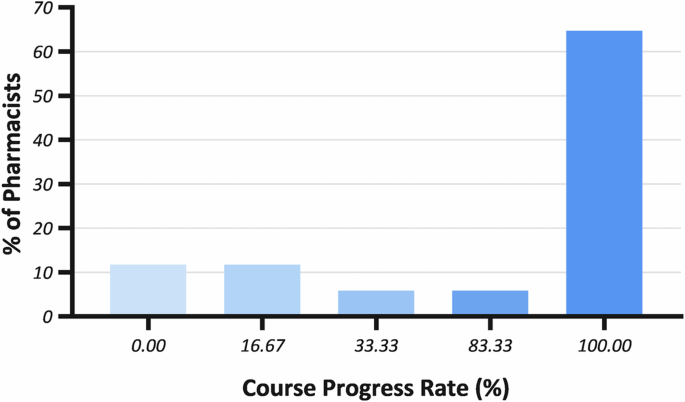
Percentages represent the proportion of pharmacists based on their completion rates of eHealthResp course modules.
Physicians’ eHealthResp online course
A total of 18 physicians explored the eHealthResp online course, while 72 physicians attended the educational intervention. Figure 3 exhibits the enrollment of physicians in the eHealthResp online course.
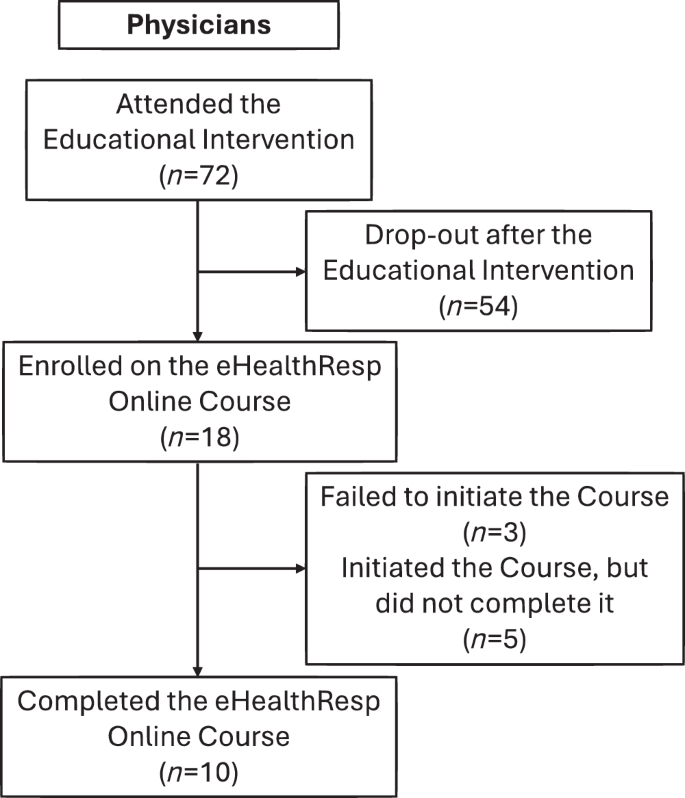
The flowchart outlines the recruitment process and course participation steps of the 72 physicians, with 18 completing the online course.
Among the physicians who engaged in the course, the average progress rate was found to be 67%. Notably, the average grade attained by the 10 physicians who completed the course was 96%, indicating a high level of engagement with the course materials. However, it is important to note that 8 physicians did not complete the course, with 3 physicians showing no progress (failed to initiate the course).
Figure 4 illustrates the progress rate of physicians in the eHealthResp online course.
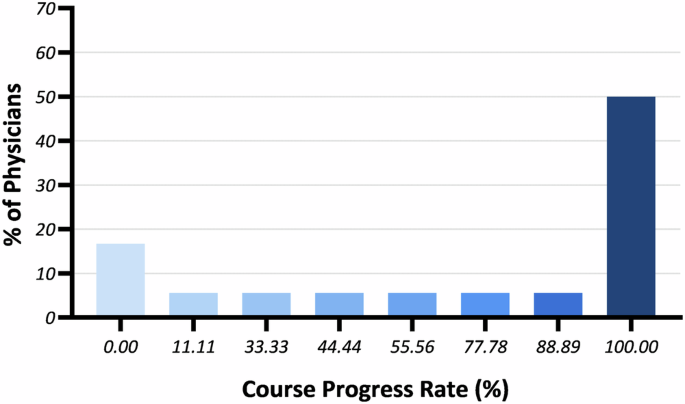
Percentages reflect the proportion of physicians based on their completion rates of eHealthResp course modules.
Pharmacists’ eHealthResp mobile app
Of the cases analysed by pharmacists through the eHealthResp mobile app, 18 searches were defined as female, 9 were defined as male, and 3 whose gender was not defined. Of these, the vast majority fell within the age range of 5 to 70 years, with only 2 below this age range and 1 above it. Table 1 presents the selected symptomatology while using the eHealthResp mobile app as well as the means and standard deviations of the intensity for several selected symptoms. The most frequently selected symptoms were acute nasal discharge, pain during swallowing, and headaches. For the duration of nasal obstruction and cough, almost all cases experienced these symptoms for less than 7 days. Notably, nasal obstruction emerged as the symptom with the highest intensity among the cases studied.
Physicians’ eHealthResp mobile app
Of the cases analysed by physicians through the eHealthResp mobile app, it was observed that 32 searches received a diagnosis without requiring further medical attention, accounting for approximately half of the cases. Additionally, 9 of the searched cases were referred for urgent otolaryngology consultation, and 5 cases were suggested for hospitalization. However, 18 out of the 64 searched cases did not have a defined response in the algorithm.
As shown in Table 2, the most common symptoms selected by physicians in the eHealthResp mobile app were nasal congestion, bulging, erythematous or opaque tympanic membrane, sensation of pressure or facial pain, and headache.
Several underlying pathologies were identified, with chronic obstructive pulmonary disease being the most common, followed by recurrent and bilateral otitis media.
Throughout the eHealthResp mobile app, inquiries were made about the exhibited clinical status, including possible exams performed, medical history, and clinical information that supported the diagnosis. Based on the obtained answers, it was possible to verify that 3 of the searched cases presented a decrease in vesicular murmur, 3 had positive results in pharyngotonsillar exudate, and other 3 presented tympanic membrane perforation.
Diagnosis
With the information provided for each of the searched cases by pharmacists/physicians using the decision support algorithm—eHealthResp mobile app –, the identified diagnoses were as follows: 11 cases of colds, 2 cases of pharyngotonsillitis, 2 cases of influenza, 1 case of acute bronchitis, and 2 possible cases of pneumonia. Moreover, 12 undetermined diagnoses were identified. Out of the 30 diagnoses obtained by pharmacists, only 4 of them had indicated the need to advise patients to consult a physician.
Among the 32 searched cases who received a diagnosis provided through the physicians’ eHealthResp mobile app without requiring further attention, it was determined that 13 had acute otitis media, 11 had acute pharyngotonsillitis, 6 had acute rhinosinusitis, and 2 had pneumonia, leaving 32 searched cases without a determined diagnosis. These results are presented in Table 3.
Discussion
This study demonstrated that the eHealthResp online course and mobile app provide information about URTIs and the corresponding protocols for their management. Considering that URTIs are the most common clinical conditions for which antibiotics are inappropriately prescribed35,36,37 in primary care settings, clinical decision support systems may be very helpful in improving antibiotic prescribing practices.
Firstly, the online course received feedback from primary care physicians and community pharmacists to address or improve some problems encountered, and secondly, the progress and scores of each group were analysed. Through the analysis of the results presented in this paper and in the previously conducted pilot studies that evaluated the healthcare professionals’ perceptions regarding these digital platforms, it was possible to conclude by the positive feedback and scores given to these e-health tools, that they contribute positively to the health literacy promotion and appropriate antibiotic prescribing for URTIs12,31,33,34. Furthermore, both the eHealthResp online course and mobile app underwent iterative development, allowing for the improvement of several parameters over time, resulting in their easy and simple use38,39.
URTIs involve organs such as the nose, pharynx, and larynx, and the most common symptoms associated with these conditions, which are the primary reason for primary care consultations40, include cough, sore throat, nasal discharge, nasal congestion, and headaches41,42. In the eHealthResp mobile app for community pharmacists and primary care physicians, the selected symptoms were aligned with these expectations, being the most common acute nasal discharge, which presented high intensity when compared to other symptoms, along with headache. Furthermore, as most selected symptoms were reported to last for less than a week, acute and self-limited infections may be the most prevalent clinical scenario for most searched cases. The majority of these URTIs usually do not require further treatment other than symptomatic relief, and the eHealthResp app suggests pharmacological and non-pharmacological therapeutic options to better manage these clinical conditions.
The symptoms commonly presented by patients and evaluated by physicians are more complex and diverse than those evaluated by pharmacists, leading to more specific diagnoses. Furthermore, the symptoms assessed by pharmacists are more common and more easily detectable than the symptoms assessed by physicians, which are characterized by a greater degree of severity, such as the presentation of bulging, erythematous, or opaque tympanic membrane12. Moreover, physicians still have access to medical history, possible exams performed, and clinical information which enables the observation of a greater number and specificity of symptoms. Despite the differences in the range of symptoms evaluated by physicians and pharmacists, the use of these e-health tools optimizes the diagnosis and prescription of antibiotics for URTIs31.
Regarding the diagnosis rates provided by the eHealthResp application, approximately 60% of searches conducted by pharmacists yielded a diagnosis, while physicians obtained a diagnosis in 50% of their searches. These figures highlight the application’s effectiveness in assisting healthcare professionals with diagnosing respiratory infections. Considering the vast array of respiratory infections and the application’s focus on the most common ones, achieving an adequate response for 40 to 50% of the cases is commendable. However, the presence of an undetermined diagnosis underscores the need to ensure that the application’s information aligns with the presented pathologies. It is crucial to emphasize that the eHealthResp application serves as a clinical decision support tool, guiding healthcare professionals with recommendations for patient care rather than providing definitive diagnosis. This distinction is essential for users to understand the application’s purpose and limitations accurately. Despite its limitations in offering conclusive diagnoses, the application’s ability to guide a significant portion of cases is a testament to its utility in clinical practice. As such, further refinement of the application’s algorithm and integration of additional clinical data could enhance its diagnostic capabilities and ultimately improve patient care outcomes.
The main limitation of this study is the sample size, as the limited number of healthcare professionals participants within the restricted timeline prevents a comprehensive understanding of the true impact on antibiotic prescriptions. However, owing to the COVID-19 pandemic restrictions, it was extremely challenging to recruit primary care physicians and community pharmacists during this period of study.
There was a lack of adherence among primary care physicians and community pharmacists to the eHealthResp clinical decision support tools, including both the online course and the mobile app. Despite the increasing recognition of digital tools as accessible and scalable solutions for improving health outcomes and promote behavior change among healthcare professionals, a significant proportion of users are not fully adhering to these tools as intended43. The average age of healthcare professionals in Portugal could be considered a limiting factor that directly influenced their adherence to digital healthcare apps and online courses, as older adults tend to have lower levels of technological proficiency, even though healthcare workers are generally considered to have higher levels of digital health literacy than the general population44. Thus, further strategies to improve adherence to these interventions should be carefully planned to avoid attrition—a particularly common phenomenon recognized in the literature regarding digital health interventions45,46.
The decision support system for pharmacists (eHealthResp app) was designed so that if the patient to whom the algorithm was applied was under 18 years old (non-adult patients), the clinical recommendation was to immediately refer the patient to a physician. This prevents the use of the algorithm for populations it was not designed for, such as pediatric patients or individuals with specific comorbidities.
Future work should aim to increase the number of healthcare professionals’ participants, enabling a more comprehensive and representative approach. Additionally, integrating these decision-support algorithms into the prescribing and dispensing processes of antibiotics for respiratory infections holds the potential for significant benefits.
Lastly, it is crucial to acknowledge the effectiveness of the educational interventions. Strengthening these interventions and promoting awareness about the proper use of antibiotics and the significance of accurate prescribing can significantly contribute to combating this issue. Understanding the impact of such interventions and developing effective strategies is an ongoing pursuit that requires cooperation and dedication from all parties involved.
In summary, the eHealthResp online course and mobile app have exhibited promising efficacy in supporting community pharmacists and primary care physicians with diagnosing and managing respiratory infections. Despite encountering limitations such as undetermined diagnoses and participant adherence challenges, these tools have shown commendable effectiveness in guiding a substantial number of cases. Future efforts should focus on increasing participant numbers and strengthening educational interventions to promote appropriate antibiotic use. Overall, these digital tools offer valuable support in clinical decision-making and have the potential to significantly improve patient care outcomes in the management of upper respiratory tract infections.
Methods
The eHealthResp project consists of an online course and a mobile application aimed at improving antibiotic use for URTIs and enhancing clinical decision-making for community pharmacists and primary care physicians32,33,34.
eHealthResp online course
The eHealthResp online course is a web platform that consists of two distinct courses, one for primary care physicians, developed with a user-centered design, and the other for community pharmacists, with both following a similar structure. The physicians’ course begins with an introduction to the course content and an overview with clinical information on several respiratory tract infections. Subsequently, six modules on specific infections (acute rhinosinusitis, acute pharyngotonsillitis, acute tracheobronchitis, acute otitis media, community-acquired pneumonia, and COVID-19) were designed, followed by four clinical cases to be solved after completing the modules. The pharmacists’ course follows the same structure however, it comprises only three modules instead of six, focusing on common cold and flu, acute rhinosinusitis, acute pharyngotonsillitis, and acute tracheobronchitis. This online course, with the main goal of supporting patients and aiding clinical decisions, ultimately aims to contribute to the improvement of respiratory infections management in primary care12,31,32,33. The progress of healthcare professionals in the eHealthResp online course was tracked by monitoring their completion of each module. Upon finishing a module, participants were required to mark it as completed, signaling their progress through the course. Subsequently, a corresponding percentage of progress was assigned, increasing proportionally with the number of completed modules. Participants who did not finish the theoretical modules were unable to proceed to the assessment module (clinical cases). After completing the assessment module, each professional received an automatic final grade, which was then used to calculate the average grade.
eHealthResp mobile application
The eHealthResp mobile app functions as a clinical decision support tool for diagnosing upper respiratory symptoms and it is available for Android and iOS mobile systems. It incorporates a total of five algorithms for physicians and four algorithms designed for community pharmacists, each addressing prevalent symptoms of URTIs on a severity scale from 1 to 5, including nasal symptoms, coughing, sore throat, and fever. These algorithms serve as the basis for supporting users towards the most probable diagnosis and appropriate therapeutic interventions, encompassing both pharmacological and non-pharmacological approaches12,31,38. The algorithms developed for physicians were formulated in alignment with implemented national47,48,49 and international50,51,52,53,54,55 clinical practice guidelines. These algorithms supported physicians in providing comprehensive advice and treatment recommendations to patients with respiratory tract disorders31, ensuring adherence to evidence-based practices. In contrast, the algorithms designed for community pharmacists were specifically oriented to support them with the necessary tools for effectively managing patients’ URTI symptoms12. By leveraging these algorithms, pharmacists can confidently guide symptom management, including recommendations for over-the-counter medication and non-pharmacological interventions. Moreover, the algorithms facilitate the identification of scenarios where further medical attention may be warranted, prompting pharmacists to refer patients to physicians for additional evaluation and treatment if necessary. In essence, the eHealthResp app operates on a simple yet effective process: it analyses the patient’s characteristics, along with the symptoms reported by the user and their intensity, to generate a proposal of diagnosis, followed by suggestions for pharmacological and non-pharmacological treatment or for medical assistance (Fig. 5).
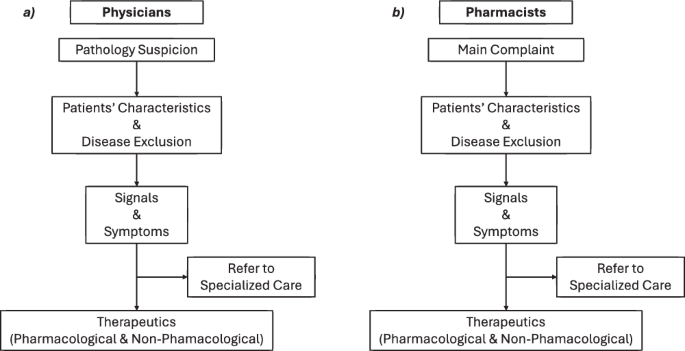
The flowchart illustrates how the algorithms for (a) physicians and (b) pharmacists analyze patient characteristics and symptoms to suggest diagnoses and treatment options, and identify scenarios requiring referral for additional medical evaluation.
Educational intervention and health professionals’ recruitment
An educational intervention was conducted in four municipalities within the Portuguese Centre Regional Health Administration (ARS-Centro) area, targeting outpatient centers and community pharmacies. This intervention, which obtained ethics approval from the Guarda Polytechnic Institute’s Ethics Committee (7/2021), occurred both in person and online during May, June, and July 2022. It aimed to familiarize primary care physicians and community pharmacists with the online course and mobile application. The recruitment process for participants involved engagement during educational interventions. Our team facilitated participant enrollment by collaborating with the College of Pharmacists, which accredited the training for participating pharmacists, and various outpatient centers of ARS-Centro. This collaborative effort ensured broad access to potential participants across different healthcare settings. Participation in the study was entirely voluntary and participants provided their informed consent before enrollment, according to the General Data Protection Regulation (GDPR).
During the educational intervention and healthcare professionals’ recruitment, our team members randomly distributed access IDs and keys to each participant. These credentials granted them access to the online course, with each user receiving unique login information. This approach ensured the prevention of duplicate registrations by the same user.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.

Responses