The combined effect of CRP and blood pressure on the risk of mortality in patients with type 2 diabetes

Introduction
In the last few decades, the prevalence and mortality of type 2 diabetes in the world have increased rapidly1,2. According to the International Diabetes Federation, the global patients with type 2 diabetes in adults has increased from 382 million in 2013 to 536.6 million in 20213,4. It was estimated that 4.2 million patients died of diabetes each year, accounting for 11.3% of global deaths5. In China, the incidence and mortality of diabetes have sharply increased6. The latest statistics reported that more than 800,000 Chinese adults aged 20–79 years died of diabetes in 20195. Therefore, it is essential to identify risk factors that are associated with the risk of mortality in diabetic patients7.
Type 2 diabetes has been regarded as an auto-inflammatory disease considering the emerging implications of inflammatory mediators in the disease progression8. C-reactive protein (CRP), an acute-phase reactive protein produced by liver in response to pro-inflammatory factors, is a sensitive biomarker for tissue injury, infection, and inflammation9. Although some studies suggest that CRP is a significant predictor of death10, others found no significant association between raised CRP and all-cause and cardiovascular mortality among type 2 diabetic patients11,12,13. On the other hand, high blood pressure (BP) has been shown an important modifiable risk factor for diabetes. A cohort study among 271,174 patients with type 2 diabetes showed that intensive blood pressure lowering treatment was associated with lower risk of death in patients with type 2 diabetes14, while no significant mortality risk was found among prehypertension compared with those without prehypertension15, and another research found an increased risk of both lower and higher BP on mortality among diabetic patients16. Considering the inconsistent findings, we examined the relationship of CRP with the risk of all-cause mortality by BP status in a cohort of Chinese type 2 diabetic population.
Methods
Study participants
Data were obtained from the China Health and Retirement Longitudinal Study (CHARLS), a nationwide longitudinal survey to evaluate the social, economic, and health status among Chinese population aged ≥ 45 years. A total of 17,707 participants were recruited from 450 communities within 150 districts in 28 provinces through probability proportional sampling method. More details of this study have been described previously17. The CHARLS study was approved by the Ethics Review Board of Peking University, and all participants provided a written informed consent.
In this study, participants with type 2 diabetes at 2011 (baseline) and participated at least one subsequent survey (2013, 2015, and 2018) were included. Sample size estimation was conducted using Schoenfeld’s formula18:
The total sample size was determined using the following formula:
With α = 0.05, β = 0.20, and P = 0.25. Given the observed mortality rate of 13.0%, the total sample size required was 638 participants.
We excluded 16,043 participants who aged < 45 years (n = 423), had missing information on CRP (n = 5864), and blood pressure (n = 1759), and did not have type 2 diabetes (n = 7997). We further excluded 33 participants who did not follow up. Finally, the study sample consisted of 1631 participants with type 2 diabetes.
Data collection
A standardized questionnaire was used to collect information on participant’s age, gender, education level (illiterate, elementary, middle school, high school, and above), marital status (married living together, married not living together, divorced/widowed/unmarried, etc.), location of residence, history of smoking (yes, no), and alcohol consumption (more than once a month, less than once a month, never drink). Participant was considered as smokers if he/she answered “yes” to the question- “Have you ever chewed tobacco, smoked a pipe, used self-rolled cigarettes, or smoked cigarettes/cigars?”. Alcohol consumption was assessed with the question- “Did you drink any alcoholic beverages, such as beer, wine, or liquor in the past year? How often?” Response options included: “More than once a month”, “Less than once a month”, and “Never drink”.
Participant’s body weight and height were measured by trained investigators. Body mass index (BMI) was calculated by dividing weight (kg) by the square of height (m2). Blood pressure was measured using Omron HEM-7200 sphygmomanometer and the average value was used for analysis. Blood glucose, high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), total cholesterol were measured by the enzymatic colorimetric test, and CRP was assayed by immuno-turbidimetric test in the clinical laboratory of Capital Medical University using fasting blood samples.
Relevant definitions
Type 2 diabetes: According to the American Diabetes Association diagnostic criteria, type 2 diabetes was defined as fasting blood glucose ≥ 126 mg/dL; and/or glycosylated hemoglobin level ≥ 6.5%19; and/or previous diagnosis of diabetes by a physician20.
Prehypertension and hypertension: Prehypertension was defined as 120 mmHg ≤ systolic BP ≤ 139 mmHg and/or 80 mmHg ≤ diastolic BP ≤ 89 mmHg. Hypertension was defined as that systolic BP ≥ 140 mmHg and/or diastolic BP ≥ 90 mmHg, or being diagnosed by a doctor, or taking antihypertensive medications. Normal BP (Normotension) was defined as systolic BP < 120 mmHg and diastolic BP < 80 mmHg, and did not use antihypertensive medication.
Mortality: At each survey wave, the participant’s status (alive or dead) was interviewed. If a participant’s death was reported, trained staff would obtain more information about the death. The survival time was calculated as the interval between the time of the first survey and the time of death.
Statistical analysis
Participants were divided into six groups according to CRP (cut-off value 3.0 mg/L) and BP status: Low CRP/normotension, Low CRP/prehypertension, Low CRP/hypertension, High CRP/normotension, High CRP/prehypertension, High CRP/hypertension.
Analysis of variance (ANOVA) or chi-square test was used to compare the difference among groups, where appropriate. Multivariate cox regression was conducted to analyze the individual and combined effects of CRP and BP status and the risk of mortality in participants. In line with previous studies on mortality in diabetic populations, several variables including age, gender, education level, marital status, location of residence, history of smoking, and alcohol consumption etc., were considered as covariates. Schoenfeld residuals was used to validate the proportional hazards assumption, and all P values for the covariates > 0.05.
To examine the effects of confounding factors, three models were constructed. Model 1: adjusted for gender and age; Model 2: Model 1 plus location of residence, education, marriage, smoking, alcohol consumption, and BMI; Model 3: Model 2 plus dyslipidemia, hypoglycemic treatment, HDL-C, and LDL-C. In addition, subgroup analyses were performed to investigate the combined effect of CRP and BP status on the risk of death in diabetic patients by gender, age, and residence. All analyses were performed using SPSS 20.0 (IBM SPSS Inc., Chicago, IL).
Results
Baseline characteristics
Table 1 shows the baseline characteristics of participants across groups. Among a total of 1631 participants, 747 (45.8%) were males, with a mean age of 60.7 ± 9.2 years at baseline. During the 7-year follow-up period, 212 (13.0%) death occurred, with the highest mortality rate in the high CRP/hypertension group (27.7%) and the lowest in the low CRP/normotension group (5.0%). The high CRP/hypertension group had the highest mean age (64.5 ± 9.4). There were statistically significant differences in education, marriage, dyslipidemia, HDL-C, CRP, and BMI among different groups (all P < 0.05).
Association of CRP and BP status with risk of all-cause mortality
Table 2 displays the association of CRP and BP status with the risk of all-cause mortality in diabetic patients. After adjustment for potential confounders (model 3), participants with high CRP (HR 1.94, 95% CI 1.45–2.61) and hypertension (HR 2.01, 95% CI 1.31–3.08) had significantly higher risk for all-cause mortality than those had low CRP/normotension.
Combined effect of CRP and BP status with risk of all-cause mortality
The Kaplan Meier plot of mortality according to CRP and BP status showed the cumulative incidence rates of all-cause mortality (Fig. 1). The survival distributions of the 6 groups were significantly different (Log-rank test P < 0.001), and participants in the high CRP and hypertension group had a higher risk of mortality compared to those in the other groups.
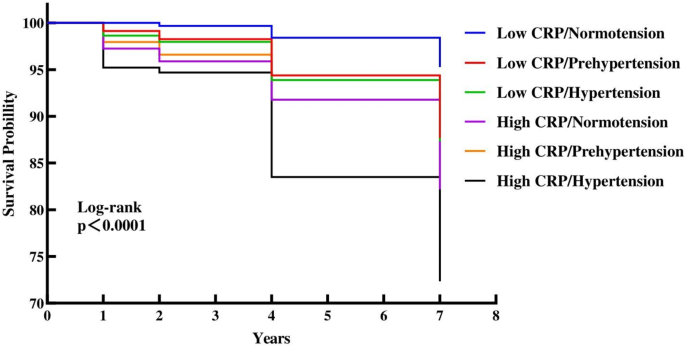
Kaplan–Meier survival curves for the all-cause mortality in six groups.
Table 3 displays the combined effect of CRP and BP status with the risk of mortality. After adjusting for several confounders, such as gender, age, education, BMI, HDL-C, and LDL-C, etc. (model 3), the respective HR (95% CI) of mortality of participants in the low CRP/prehypertension, low CRP/hypertension, high CRP/normotension, high CRP/prehypertension, high CRP/hypertension group were 1.97 (1.12–3.48), 2.19 (1.24–3.88), 3.50 (1.67–7.33), 2.03 (1.00–4.09), and 4.79 (2.68–8.57), compared with the low CRP/normotension group.
Subgroup analysis by gender, age, and residence
Subgroup analysis by participants’ gender, age, and residence is shown in Table 4. Participants in the high CRP/hypertension group had the highest risk of mortality after adjusting for several potential confounders, and the risk was especially high in those < 60 years old (HR 5.48, 95% CI 1.83–16.4), men (HR 4.91, 95% CI 2.28–10.57), and those who lived in the rural district (HR 6.09, 95% CI 2.83–13.12).
Discussion
In this 7-year prospective cohort study, we found significantly increased risk of all-cause mortality among type 2 diabetic patients with high CRP and hypertension, in comparison with their counterparts. Furthermore, the combination of high CRP and hypertension were associated with the highest risk of mortality.
CRP is one of the first acute-phase proteins synthesized and released in the liver. Researchers have widely used CRP to evaluate the severity of acute injury and inflammation in vivo. Previous studies suggest that elevated CRP was an independent predictor of all-cause mortality in the general population21, but the results were inconsistent among diabetic patients11,12. Our results provide more evidence showing that high levels of CRP conferred an increased risk of mortality in middle aged and elderly Chinese diabetics. The gender differences in the associations we observed have also been reported previously. A meta-analysis of 22 cohort studies among 484,821 general participants found that high CRP levels were significantly associated with the risk of mortality among men22, but not among women, compared with low CRP levels. While endogenous hormones might explain the different gender effects on the relationship of CRP with death risk23, the optimal thresholds of CRP for risk stratification remain to be explored in future studies.
High BP is one of the global leading mortality predictors. Hypertension and diabetes have been shown to share common risk factors, thus commonly occur in individuals. In line with previous studies that documented associations between hypertension and death among the general population, we found high BP (prehypertension and hypertension) significantly increased the risk of mortality in diabetic patients. In addition, our study provides evidence that there was combined effects of CRP and high BP on the risk of all-cause mortality among diabetic population. The underlying mechanisms by which CRP and high BP were linked to mortality might have several explanations. One reason is that high BP increased the risk of death through its negative effects on several target organs, including heart, brain, and kidney, leading to structural and functional damages, such as wall hypertrophy, atheromatous lesions, and calcification24. On the other hand, hyperglycemia in diabetic patients can trigger increased CRP concentrations, which reflect the stress and inflammation state of the body. Furthermore, CRP may be involved in the development of atherosclerosis by promoting thrombosis, resulting in ischemia–reperfusion injury25. Thus, high CRP and high BP can synthetically provide a positive effect to increase the risk of death.
This study has several strengths. Most previous investigations have primarily focused on Western populations. Although one study reported the relationship between CRP and mortality in a Chinese hyperglycemia sample, only 286 participants were recruited from Da Qing city, China26. In contrast, our study comprised 1631 Chinese participants, representing a large-scale and nationally representative cohort. Furthermore, previous studies only examined the individual factor (CRP or BP) with mortality, while our study investigated the combined effect of CRP and BP on mortality risk, thereby offering an important public health and clinical insight, thereby offering an important public health and clinical insight.
However, some limitations should be acknowledged. First, CRP concentrations and BP were only measured at baseline, so it remains unclear whether the relationships would have been affected by CRP and BP changes over time. Second, the association between CRP, BP and cause-specific death cannot be examined because the specific reason for death was not available in CHARLS. Third, although several important variables have been adjusted, some unmeasured confounding factors might still exist. Finally, only middle-aged and elderly Chinese adults have been included in this study, therefore our results may not be generalizable to other population.
In conclusion, this study showed that high CRP, BP and their combinations were significantly associated with an increased risk of all-cause mortality in Chinese type 2 diabetic patients. Therefore, effective interventions aiming at lower CRP and BP are warranted to reduce the risk of all-cause mortality in this population.




Responses